If you’re having the same nightmare over and over, let me say this upfront: you’re not “crazy,” you’re not broken, and your brain isn’t being dramatic for attention.
Recurring nightmares are often what happens when your brain has emotions or fear stuff it hasn’t fully processed… so it tries again. And again. And again. Like it’s refreshing the worst tab in your mental browser at 3:07 a.m.
The short answer: Recurring nightmares are common, and they often improve when you reduce sleep disruption, identify triggers (stress, trauma, meds, substances), and practice a proven technique like Imagery Rehearsal Therapy (IRT)/rescripting for a few weeks [Augedal et al., 2013].
Key exception: If you might have sleep apnea, REM sleep behavior disorder (acting out dreams), PTSD related nightmares, or new nightmares after starting/changing meds get evaluated rather than trying to “DIY” it indefinitely [AASM ICSD-3].
When it matters less: If you have a rough patch of stress dreams for a week or two and they fade as life calms down, that’s usually not a sign something is “wrong.”
I’ve been there. I went through a stretch where I kept dreaming I was back in school late to an exam, no pants (why is that always the detail?), and everyone was judging me like they were paid to do it. I had not been in school for YEARS. Which is how I figured out: okay, this isn’t about a pop quiz. This is about anxiety wearing a trench coat and pretending to be “Dream Logic.”
Let’s talk about what’s actually going on, what’s secretly making it worse, and what you can do starting tonight.
First: Is it a “recurring nightmare” or just a stress dream doing the most?
Not every bad dream that repeats once or twice is a whole thing.
- Stress dreams are like temporary pop up ads. They show up when life is loud (big presentation, family drama, money stress), then fade when things calm down.
- Recurring nightmares are patterns disturbing dreams that repeat and cause distress, sleep avoidance, or daytime impairment. Clinically, “nightmare disorder” is diagnosed based more on distress/impairment + frequency (and ruling out substances/other sleep disorders) than on one magic timeline [AASM ICSD-3].
A decent rule of thumb (not a diagnosis): if the dream is still showing up most weeks for ~a month, or it’s making you dread sleep, it’s worth addressing more directly (and possibly getting help).
How to stop recurring nightmares (a prioritized plan)
If you’re here for the “just tell me what to do” part, this is the triage path many sleep clinicians use.
Tonight (10 minutes)
- Reduce “nightmare lock in” awakenings: do a quick wind down, keep the room dark/cool/quiet, and avoid alcohol close to bedtime (more on why below).
- Do the one word emotion note when you wake (you’ll see it later in this article).
- If you’re too activated to sleep: get out of bed briefly, do a calm reset (dim light, slow breathing, neutral reading), then return when sleepy. This reduces the bed=panic connection (a CBT-I principle) [AASM Behavioral Tx Guideline, 2021].
This week (30-60 minutes total)
- Check for “fixable” triggers: new meds, cannabis/alcohol changes, sleep deprivation, irregular schedule, overheating, stress spike.
- Screen yourself for red flags (apnea, acting out dreams, trauma symptoms). If they’re present, skip ahead to “When to get professional help.”
Over 2-6 weeks (the “this actually changes the pattern” phase)
- Practice IRT/rescripting daily (5-10 minutes) for at least 2 weeks many people who respond notice improvement over several weeks [Augedal et al., 2013].
- If insomnia is part of the picture: consider CBT-I (not just sleep tips). Treating insomnia can reduce awakenings that make nightmares more memorable [AASM Behavioral Tx Guideline, 2021].
- If trauma is involved: consider trauma focused therapy (and/or a clinician trained in IRT for trauma nightmares). Trauma linked nightmares often need more than generic stress management [VA/DoD PTSD Guideline, 2023].
Quick note: This article is education, not medical care. If you’re dealing with trauma, self-harm thoughts, or a sleep disorder, you deserve real support not just internet coping.
Why your brain keeps hitting replay (rude, but explainable)
During REM sleep (when a lot of vivid dreaming happens), the brain’s emotional systems are active, and the “context + regulation” systems may be less online than they are during the day which is one reason dreams can feel intense and bizarre [Walker & van der Helm, 2009]. For some people, dreaming seems to be part of emotional processing and memory integration, but the science is still evolving and not everyone’s nightmares have one single cause [Walker & van der Helm, 2009].
And if you wake up in a panic? That surge of emotion can make the dream more memorable, which may make it easier for your brain to replay it.
Three common loop boosters:
- Long term stress / hyperarousal: When your nervous system is running hot, fear based dreams can ramp up.
- Trying not to think about it: Thought suppression can backfire (the “pink elephant” effect).
- Fragmented sleep: If you’re waking up a lot (insomnia, sleep apnea, etc.), it’s easier for nightmares to get “locked in” and remembered [AASM ICSD-3].
The sneaky triggers that keep nightmares going
This is the part where I gently suggest you put on your detective hat but like, a comfy one.
1) The thing you’re avoiding in real life
Recurring nightmares often orbit around unresolved stress: a conversation you’re not having, a decision you’re not making, grief you’re trying to outrun, a boundary you keep swallowing.
And yes sometimes the nightmares ease when you address the underlying stressor. Not always, not instantly, and not as a moral reward for “being brave.” But it can matter.
2) Anxiety + self-criticism (your inner bully, now in IMAX)
Anxiety is commonly linked with more frequent nightmares, and harsh self-talk can keep your brain in threat mode especially if your days are heavy on “I’m failing” / “I’m behind” / “I’m not enough.” (It makes sense if your dreams show up as being chased, unprepared, exposed, or out of control.)
3) Sleep quality (aka: if sleep is wobbly, dreams get weird)
When sleep is unstable, nightmares often increase. Insomnia is a big one. Also, both too little sleep and irregular sleep timing can correlate with more vivid dreaming and more awakenings meaning more chances to remember a nightmare [AASM ICSD-3].
Real talk: your brain likes a steady runway. Turbulence makes everything bumpier.
4) Medications + substances (worth checking, not worth panicking)
If nightmares started after a new medication or after a dose change talk to your prescriber or pharmacist. Don’t stop meds abruptly.
Some medications are reported to affect dreaming or increase vivid dreams/nightmares in some people, depending on the specific drug, dose, timing, and your sleep architecture. Examples can include certain antidepressants (including SSRIs/SNRIs), beta blockers, stimulants, and sedating antihistamines but the effect is variable, and sometimes the same medication improves sleep overall [Wichniak et al., 2017].
Also: alcohol can reduce REM earlier in the night and contribute to more REM later (“REM rebound”) as it wears off, which may increase vivid dreams and sleep disruption in some people [Roehrs & Roth, 2001]. If this might be you, consider avoiding alcohol within ~4-6 hours of bedtime and see what changes. (No perfection required just useful data.)
If you use cannabis: some people notice changes in dream vividness with use, reductions, or stopping so if your pattern changed around a cannabis shift, that’s worth noting too. If you’re using any substance to sleep, it’s a good topic for a clinician, because sleep benefits and side effects can trade places over time.
5) Physical sleep issues (please don’t skip this part)
Before you decide this is “all psychological,” it’s smart to rule out physical factors.
- Obstructive sleep apnea (OSA) can fragment sleep and is associated in some studies with nightmares or distressing dreams for certain people especially when sleep is repeatedly interrupted (look for loud snoring, witnessed pauses, gasping, morning headaches, and daytime sleepiness) [AASM ICSD-3].
- If you act out dreams (thrashing, punching, yelling, jumping out of bed), that can signal a parasomnia like REM sleep behavior disorder (RBD), which deserves prompt medical evaluation especially if injuries are possible [AASM ICSD-3].
Who should be extra careful (quick edge case notes)
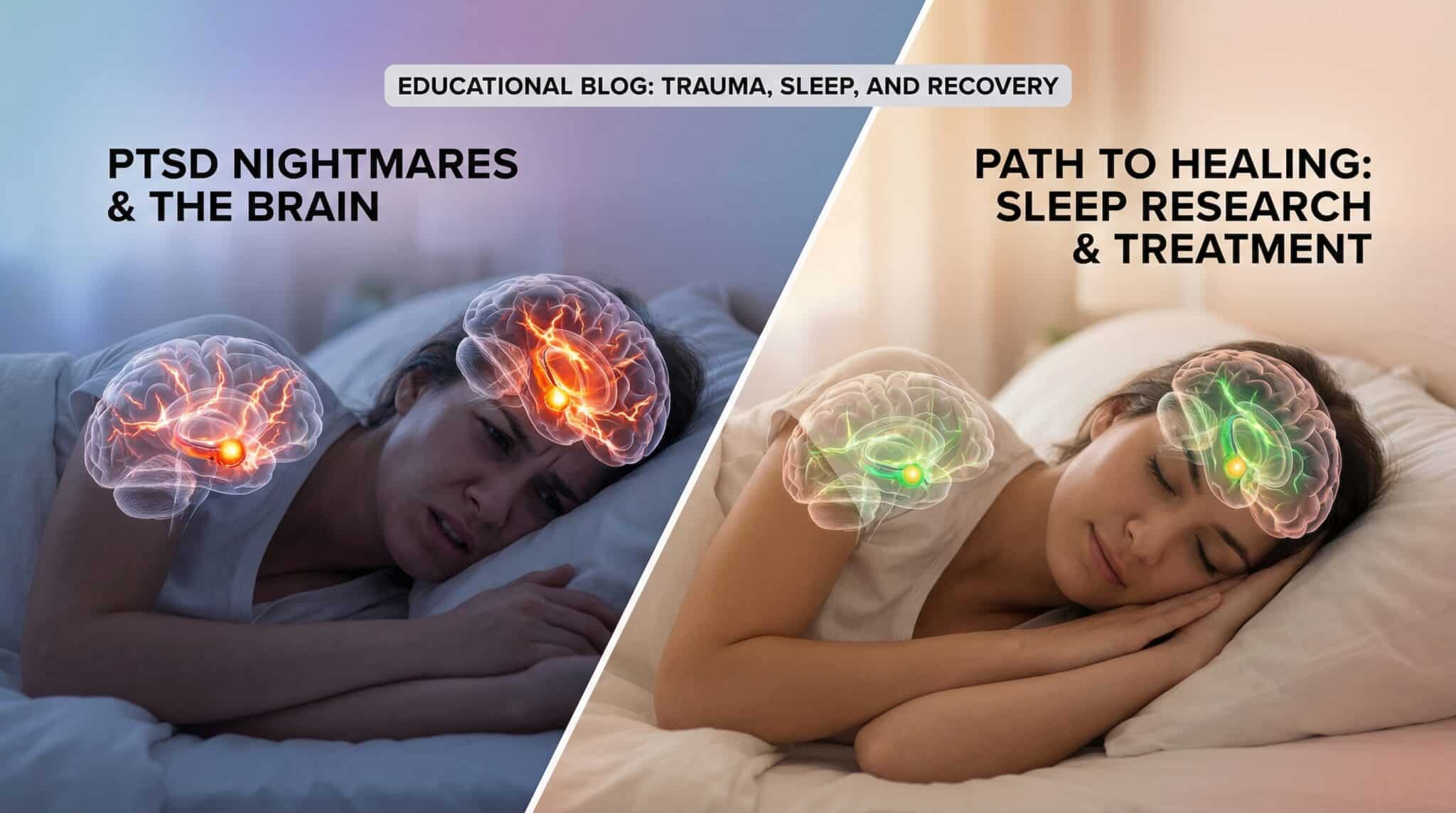
- If you have trauma/PTSD symptoms: nightmares may be part of a broader pattern (hypervigilance, flashbacks, avoidance). Trauma focused care and/or IRT with a trained clinician can be especially helpful [VA/DoD PTSD Guideline, 2023].
- If you might have sleep apnea: don’t white knuckle it treating OSA can improve sleep fragmentation and may reduce nightmare burden for some people [AASM ICSD-3].
- If you act out dreams (possible RBD): prioritize a sleep evaluation. This isn’t a “just meditate more” situation, and safety steps (padding, removing hazards) matter while you wait [AASM ICSD-3].
- If you’re pregnant/postpartum: vivid dreams and sleep disruption are common, and new/worsening nightmares can happen. If you’re also experiencing significant anxiety, depression, or intrusive thoughts, it’s worth bringing up early with your OB/midwife or primary care clinician.
- If you’re a parent reading for a child/teen: nightmares are common in kids, but frequent nightmares with daytime distress, trauma exposure, or sleepwalking/acting out behaviors should be discussed with a pediatric clinician.
Common nightmare “plots” (and what they often point to)
Dream symbols aren’t universal. A tsunami dream doesn’t have one official meaning like it’s in the Dream Dictionary Constitution.
But some themes show up a lot:
- Being chased/attacked: avoidance, conflict, looming decision
- Falling: feeling out of control, instability, major transitions
- Late/unprepared: perfectionism, fear of judgment, pressure
- Teeth falling out: loss of control, identity shifts, big life changes
- Death/dying: grief, fear, major endings/beginnings
The key isn’t the plot it’s the emotion. Fear, shame, helplessness, panic, disgust… that’s the breadcrumb trail.
What to do tonight (a small plan that actually helps)
You don’t need to “solve your entire life” before bedtime (please don’t try bedtime is not the time for a personal reinvention montage).
Here’s the simplest first step I recommend:
Step 1: Write down ONE word when you wake up
Keep a notepad by your bed. When you wake from the nightmare, write the main emotion in the first two minutes.
Not the whole plot. Not a ten page analysis. Just: fear or shame or trapped or even WHAT.
That one word is wildly useful.
Step 2: Ask one question in the morning
Later (in daylight, with caffeine), ask:
“Where do I feel this exact emotion in my real life right now?”
Not “What does it mean that there were clowns and a staircase?” Just: where is this feeling living in your day to day?
The technique that helps a lot of people: rescripting (aka: changing the ending)
If you want the most practical at home strategy for recurring nightmares, this is it: rescripting, often used in Imagery Rehearsal Therapy (IRT) a well studied behavioral approach for nightmare reduction [Augedal et al., 2013].
Here’s the DIY friendly version:
- Write the nightmare down (once, during the day).
- Pick a moment where the dream could shift.
- Rewrite it with a realistic change.
Not “I sprout wings and fly away.” More like: “I notice a door,” “I call someone,” “I turn on the light,” “I tell the person to stop,” “I leave.”
- Rehearse the new version for 5-10 minutes daily for 2-6 weeks. (Many protocols use daily practice. Response time varies.) [Augedal et al., 2013]
It can feel silly. Your brain does not care. Your brain loves repetition so give it a better script to repeat.
Important: If writing/rehearsing the nightmare spikes distress, causes panic, or you feel dissociated or unsafe, stop and get professional support.
What helps most (and what to watch for): a quick table
| Strategy | What you do | Evidence strength | Best for | Watch out for |
|—|—|—|—|—|
| IRT / rescripting | Rewrite + rehearse a safer ending daily | Promising to strong (multiple trials/meta analyses) [Augedal et al., 2013] | Recurrent nightmares, including trauma linked | Stop if it triggers overwhelm/dissociation. Consider clinician support |
| CBT-I (for insomnia) | Treat insomnia drivers + reduce conditioned arousal | Strong for insomnia. May indirectly reduce nightmares by reducing awakenings [AASM Behavioral Tx Guideline, 2021] | Nightmares + insomnia | DIY tips help, but formal CBT-I is often more effective |
| Screen/treat OSA | Sleep study, CPAP/oral appliance as indicated | Well established for apnea. Nightmare impact varies [AASM ICSD-3] | Snoring, gasping, daytime sleepiness | Don’t self-diagnose get evaluated |
| Medication/substance review | Review timing/dose/alternatives with prescriber | Mixed/variable (depends on drug) [Wichniak et al., 2017] | New or worsening nightmares after med/substance change | Don’t stop meds abruptly. Avoid stigmatizing yourself |
| Trauma focused therapy | Evidence based trauma care (e.g., CPT/EMDR), often plus sleep work | Strong for PTSD symptoms. Nightmares may improve [VA/DoD PTSD Guideline, 2023] | PTSD symptoms, trauma related nightmares | Choose a trauma informed clinician. Pacing matters |
The boring basics that help more than they should
I know, I know. Everyone wants the interesting answer. But the “boring” sleep stuff matters because it reduces awakenings, and fewer awakenings often means fewer remembered nightmares [AASM ICSD-3].
A few that actually move the needle:
- Keep sleep/wake times within ~30-60 minutes day to day (yes, even weekends sorry).
- Create a short wind down routine (20-30 minutes of “we are powering down now”).
- Keep your room cool and comfortable. Many sleep orgs recommend a cool bedroom around 60-67°F (15.6-19.4°C), but comfort varies use it as a starting range, not a rule [National Sleep Foundation].
You’re not trying to become a perfect sleeper. You’re trying to give your brain a less chaotic stage.
When you should get professional help (because sometimes DIY isn’t the move)
Consider getting evaluated for nightly distressing dreams if you have:
- nightmares that happen weekly (or more) and persist for a month or longer, especially with distress or impairment [AASM ICSD-3]
- sleep avoidance, significant anxiety about bedtime, or daytime sleepiness that affects work/school/safety
- nightmares clearly tied to trauma, or other PTSD symptoms [VA/DoD PTSD Guideline, 2023]
- signs of sleep apnea (snoring, gasping, witnessed pauses) or dream enactment behaviors [AASM ICSD-3]
Seek urgent help if nightmares come with suicidal thoughts, self-harm urges, hallucinations, or severe dissociation, or if you feel unsafe.
If you’re in the U.S., you can call or text 988 (Suicide & Crisis Lifeline). You can also text HOME to 741741 (Crisis Text Line).
If nightmares are trauma linked, a trauma informed therapist (and/or a clinician trained in IRT/CBT for nightmares/CBT-I for insomnia) can be a game changer. There are also medications that may help in specific cases (for example, prazosin has been used for PTSD related nightmares, though evidence has been mixed and individualized decision making matters) [VA/DoD PTSD Guideline, 2023].
Frequently Asked Questions
Why do recurring nightmares happen in the first place?
Recurring nightmares often show up when your sleep is fragmented, your stress system is “on,” or your brain is stuck rehearsing fear. They can also be linked with trauma, anxiety, certain medications/substances, or sleep disorders like apnea. The pattern matters most when it causes distress, sleep avoidance, or daytime impairment [AASM ICSD-3].
Are recurring nightmares a sign of PTSD?
They can be, but not always. PTSD related nightmares are often accompanied by other symptoms (avoidance, hypervigilance, intrusive memories, mood changes). If you suspect PTSD especially after a traumatic event getting trauma informed support is a strong next step [VA/DoD PTSD Guideline, 2023].
Can anxiety cause recurring nightmares?
Yes anxiety and chronic stress are commonly associated with more nightmares and more awakenings, which makes nightmares more likely to be remembered and repeated. That doesn’t mean “it’s all in your head” in a dismissive way. It means your nervous system may need support both day and night.
How long does Imagery Rehearsal Therapy (IRT) take to work?
Many IRT style protocols use daily practice for several weeks, and some people notice improvements within 2-6 weeks (response varies). It tends to work best when you rehearse consistently and pair it with better sleep stability [Augedal et al., 2013].
What should I do right after I wake up from a nightmare?
First, orient yourself: remind your brain you’re safe (look around the room, name a few objects). Then do something small and grounding slow breathing, a sip of water, dim light before trying to fall back asleep. If you want data, jot down one emotion word so you can work with it later.
Can alcohol, weed, or melatonin make nightmares worse?
Alcohol can disrupt sleep and contribute to vivid dreaming later in the night for some people [Roehrs & Roth, 2001]. Cannabis changes dreaming for many people (sometimes fewer dreams, sometimes rebound vivid dreams with reduction/cessation). Melatonin can increase dream vividness in some, but effects vary if nightmares started after a new supplement, pause and discuss it with a clinician.
When should I see a doctor or sleep specialist for nightmares?
See a clinician if nightmares are weekly for a month, cause sleep avoidance or daytime impairment, if you snore/gasp or feel dangerously sleepy in the day, or if you act out dreams (thrashing, punching, leaving the bed). Get urgent help if you have suicidal thoughts, self-harm urges, hallucinations, or severe dissociation.
Take back bedtime, one small step at a time
Recurring nightmares aren’t a character flaw. They’re a signal sometimes emotional, sometimes physical, sometimes both that something needs attention.
Start small:
- one emotion word on paper,
- one pattern noticed,
- one simple rescript practiced,
- one sleep habit stabilized.
You don’t have to accept nightly reruns forever. Your brain may be trying to process something. You can help it do that without being terrorized at 3 a.m.
Sources
- American Academy of Sleep Medicine. International Classification of Sleep Disorders (ICSD-3). AASM, 2014. (diagnostic manual)
- Augedal AW, Hansen KS, Kronhaug CR, Harvey AG, Pallesen S. “Randomized controlled trials of psychological and/or pharmacological treatments for nightmares: a meta analysis.” Sleep Medicine Reviews, 2013. (meta analysis)
- Riemann D, Baglioni C, Bassetti C, et al. “European guideline for the diagnosis and treatment of insomnia.” Journal of Sleep Research, 2017. (guideline/overview)
- Edinger JD, Arnedt JT, Bertisch SM, et al. “Behavioral and psychological treatments for chronic insomnia disorder in adults: an American Academy of Sleep Medicine clinical practice guideline.” Journal of Clinical Sleep Medicine, 2021. (guideline)
- Walker MP, van der Helm E. “Overnight therapy? The role of sleep in emotional brain processing.” Psychological Bulletin, 2009. (review)
- Wichniak A, Wierzbicka A, Jernajczyk W. “Sleep and antidepressant treatment.” Current Psychiatry Reports, 2017. (review)
- Roehrs T, Roth T. “Sleep, sleepiness, and alcohol use.” Alcohol Research & Health, 2001. (review)
- U.S. Department of Veterans Affairs / Department of Defense. VA/DoD Clinical Practice Guideline for the Management of Posttraumatic Stress Disorder and Acute Stress Disorder. 2023. (guideline) https://www.healthquality.va.gov/guidelines/MH/ptsd/
- National Sleep Foundation. “Bedroom temperature for sleep.” (overview) https://www.thensf.org/what-is-the-best-temperature-for-sleep/