Last updated: 2025-12-23
For education only. This is not medical advice and can’t diagnose you.
If your brain is hosting a nightly horror film festival and you did not buy tickets—hi, welcome. Nightmares are way more common than most people admit out loud (because nobody wants to be the person at brunch saying, “So anyway, I was being chased by faceless wolves again…”).
The short answer: Nightmares “every night” are often linked to stress, sleep disruption, substances/withdrawal, medications, or sleep disorders and many improve once you identify (and remove) the trigger.
Key exception: If you’re acting out dreams, having suicidal thoughts, or symptoms suggest sleep apnea or REM behavior disorder, get evaluated promptly.
When it matters less: An occasional nightmare especially during stress, illness, or after a scary show usually isn’t a sign anything is “wrong.”
Key takeaways (save you a scroll):
- Nightmares happen most often in late night REM sleep, which is why they love the 4-7 AM window [AASM Sleep Education: Sleep Stages & REM].
- “Nightmares every night” is a frequency clue, not a character flaw—track timing + triggers for 1-2 weeks.
- Common, fixable drivers: sleep deprivation/REM rebound, alcohol/cannabis changes, late caffeine, and medication timing [Mayo Clinic: Nightmares; AASM Sleep Duration Consensus].
- Sleep apnea can contribute to scary awakenings for some people—especially with loud snoring + daytime sleepiness [AASM: OSA overview].
- Imagery Rehearsal Therapy (IRT) is a first line, evidence based treatment for recurrent nightmares, including trauma related nightmares [Aurora et al., 2010 (AASM best practice guide)].
- Prazosin may help PTSD related nightmares for some people, but evidence is mixed and it requires prescriber guidance (blood pressure effects) [VA/DoD PTSD CPG, 2023; Raskind et al., 2018].
- If nightmares are frequent and impairing, clinicians may evaluate for nightmare disorder (and look for underlying sleep/mental health causes) [ICSD-3].
Here’s the thing I want you to hear right away: nightmares are usually signals, not life sentences. They’re your brain waving a giant neon flag that says, “HELLO, SOMETHING IS OFF,” and the good news is… a lot of those “somethings” are fixable. Sometimes it’s stress. Sometimes it’s a medication timing thing. Sometimes it’s your sleep schedule doing chaotic gremlin behavior. And yes—sometimes it’s your airway.
Let’s troubleshoot this like adults who are tired of waking up at 4:37 AM with a racing heart and a deep desire to sage the entire bedroom.
The “Don’t Overthink It” Nightmare Game Plan
I’m not going to tell you to “think positive thoughts” and sprinkle lavender on your pillow like we’re summoning the Sleep Fairy. We’re doing an actual plan:
- Check for safety/urgency first. If you’re at risk of harming yourself, or you’re acting out dreams, that’s a “get help now” situation.
- Knock out the common, fixable triggers. Sleep schedule, alcohol/cannabis changes, caffeine timing, meds, possible sleep apnea—these are the usual suspects.
- If it’s still happening, match the fix to the cause. Trauma linked or chronic nightmares often respond best to specific therapies (and sometimes medication), not just “better vibes” [Aurora et al., 2010; VA/DoD PTSD CPG, 2023].
Sticky-note truth: nightmares are information. Annoying information. But still information.
A quick definition (because “every night” usually means you want something concrete)
Clinicians may consider nightmare disorder when nightmares are recurrent, cause distress or daytime impairment, and aren’t better explained by substances/withdrawal, medications, or another sleep disorder [ICSD-3]. Research studies often use “about weekly or more” as a practical threshold, but what matters most is impact (sleep avoidance, anxiety about bedtime, daytime functioning).
Why Nightmares Love 4-7 AM (Because of Course They Do)
Your sleep isn’t one long flat nap. It cycles—and REM sleep (the stage where vivid dreaming is most common) shows up more in the last chunk of the night [AASM Sleep Education: Sleep Stages & REM]. That’s why so many people get slammed with nightmares between about 4 and 7 AM.
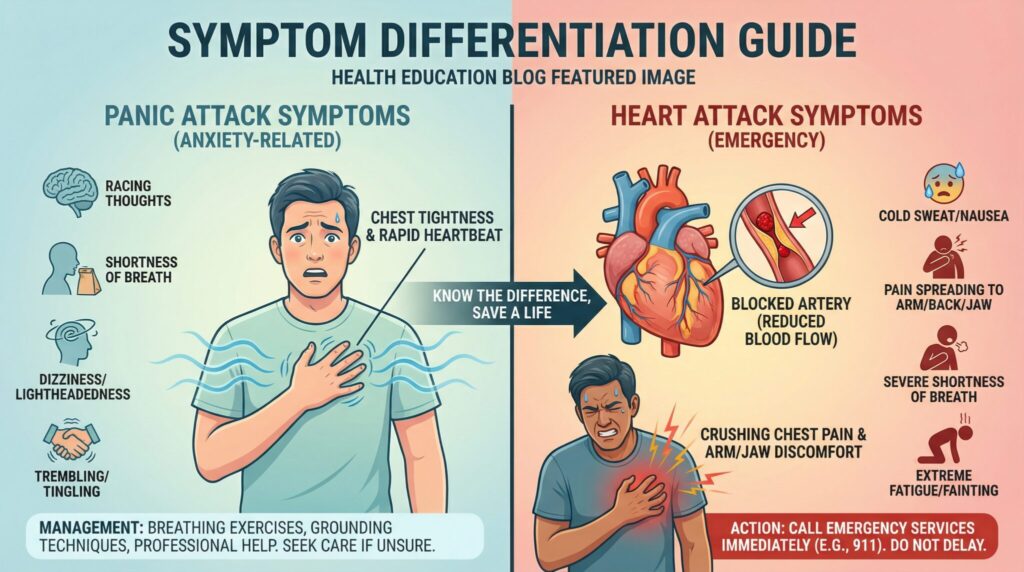
This timing matters because not every “scary night thing” is a nightmare:
- Nightmare: You wake up fully alert and can usually describe the dream in horrifying detail. (Congrats?)
- Night terror: Often earlier in the night, lots of thrashing/panic, but you might not remember a dream.
- Sleep paralysis: You wake up and can’t move for a short time. Terrifying, usually harmless, and very rude.
- REM Behavior Disorder (RBD): You act out dreams—kicking, punching, jumping up. This can cause injuries and needs medical evaluation; it’s also associated with a higher risk of certain neurodegenerative conditions in adults, so it’s not something to shrug off [Postuma et al., 2019 (review); AASM: Parasomnias/RBD overview].
Tonight, if you wake up from a nightmare, do one tiny detective thing: note roughly what time it happened. Don’t write a novel at 4 AM—just clock the pattern.
Okay, So What’s Actually Triggering Your Nightmares?
Nightmares are rarely random. They’re more like smoke alarm dreams: loud, dramatic, and technically trying to help… while also making you want to rip the batteries out.
1) Sleep apnea (yes, really)
This one gets missed a lot. If your breathing is repeatedly interrupted during sleep, it can fragment sleep (including REM), and some people report more distressing dreams or awakenings with choking/suffocating themes [AASM: OSA overview].
Clues to pay attention to:
- loud snoring
- daytime sleepiness (especially if it affects driving or work)
- someone has witnessed you stop breathing/gasp in sleep
If any of that is you, talk to your primary care doctor about screening for sleep apnea before you decide your brain is “just broken.” Sometimes it’s not your mindset it’s your airway.
2) Your medications (or when you take them)
Nightmares can show up days to weeks after starting, stopping, or changing certain medications. Some commonly reported culprits include:
- SSRIs/SNRIs (like sertraline or venlafaxine)
- beta blockers (like propranolol)
- nicotine patches
- stimulants taken too late
Medication effects vary by person, dose, and timing [Mayo Clinic: Nightmares]. If your nightmares started within a week or two of a med change, talk to your prescriber or pharmacist. Sometimes adjusting timing (morning vs. night) or dose can help—without you having to overhaul your entire bedtime routine.
Important: don’t stop a prescription medication abruptly unless a clinician tells you to. Some medications require tapering.
3) Sleep deprivation + REM rebound (aka your brain catching up)
When you don’t get enough sleep, your body may “prioritize” REM later—often called REM rebound—which can mean more vivid dreams and, for some people, repeating bad dreams [AASM Sleep Education: Sleep Deprivation/REM].
If your schedule has been chaotic, try this like it’s an experiment: aim for a consistent 7-9 hours (whatever is realistic for your life) for 2-3 weeks [AASM/SRS Sleep Duration Consensus, 2015]. Not forever. Just long enough to see what happens when your brain isn’t running on fumes.
Think of sleep like charging your phone. Let it hit 2% for days and it starts doing cursed things. Your brain can too.
4) Alcohol, cannabis changes, and caffeine sneakiness
I’m not here to take your fun away. I am here to tell you that your “nightcap” might be wearing a little “nightmare fuel” name tag.
- Alcohol: can disrupt sleep architecture and lead to more awakenings later in the night (when REM is heavier), which may make nightmares more likely for some people [NIAAA: Alcohol and Sleep (overview)].
- Cannabis: some people report vivid dreams/nightmares when cutting back or stopping after regular use (withdrawal can be a factor) [NCCIH: Cannabis (overview)].
- Caffeine: it hangs around; late day caffeine can worsen sleep onset and fragmentation in sensitive people [AASM Sleep Education: Caffeine & Sleep].
If nightmares are frequent, try a 2-3 week “cleaner” stretch: earlier caffeine, no alcohol close to bedtime, and note any cannabis changes. You’re not making a moral choice—you’re collecting data.
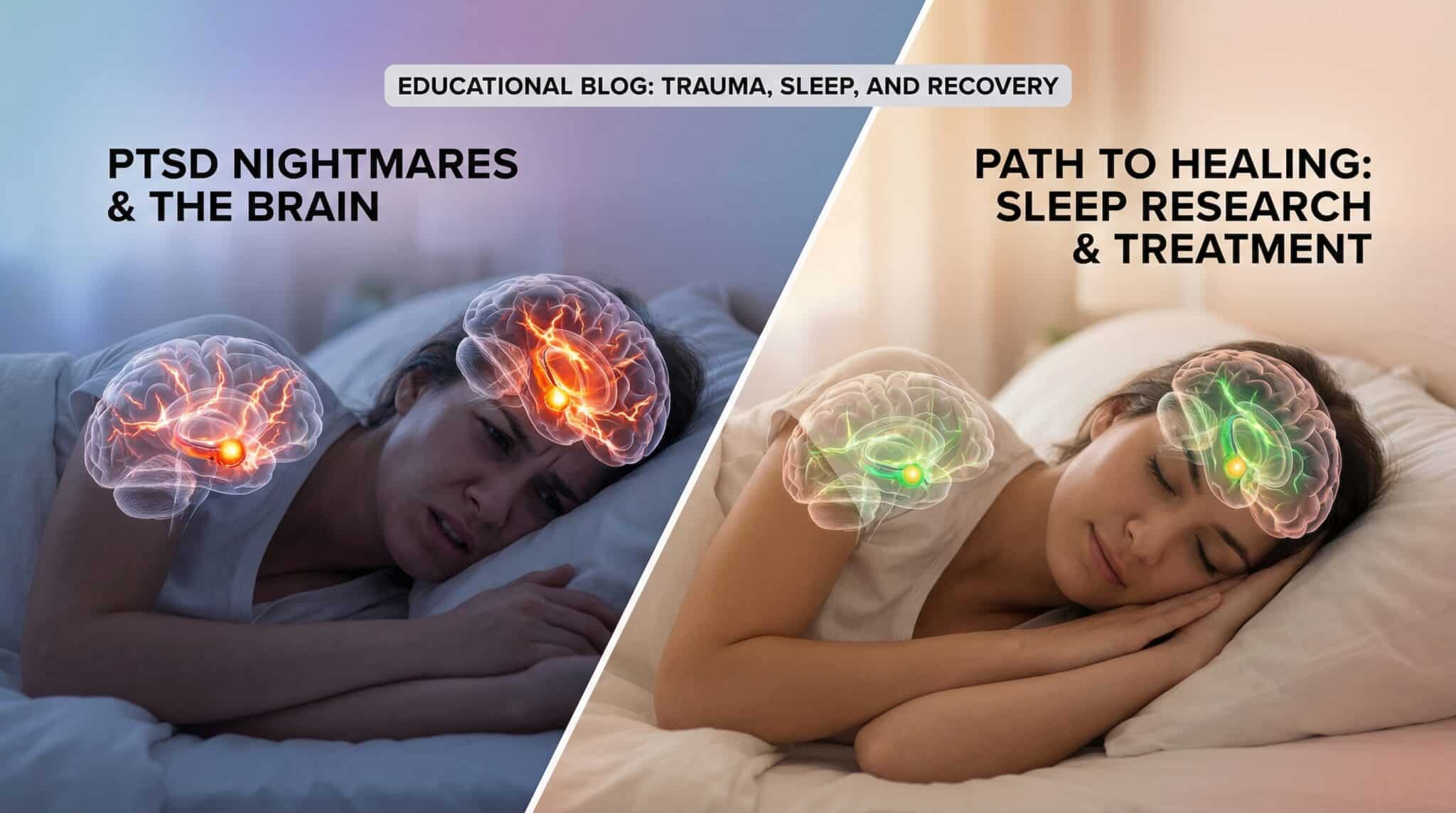
5) Stress, anxiety, depression, trauma
Stress doesn’t always show up as “I feel stressed.” Sometimes it shows up as “I keep dreaming I’m trapped in an Ikea and all the exits are blocked by my unfinished to do list.”
Trauma linked nightmares can be especially persistent and distressing. If this fits you, there are treatments that can help—this is not a “just relax” situation [APA: PTSD Treatments (overview); VA/DoD PTSD CPG, 2023].
Other Common Causes People Search for (And Yes, They Count)
If your nightmares feel sudden, nightly, or “why now?,” these are worth a quick check:
- Fever/illness: being sick (especially with fever) can make dreams more vivid and disturbing for some people [Mayo Clinic: Nightmares].
- Pregnancy/postpartum: sleep fragmentation, anxiety, and hormonal shifts can intensify dreams; if you’re also feeling depressed, panicky, or unable to sleep, bring it up at prenatal/postpartum visits (you deserve support).
- Blood sugar swings (especially diabetes): nighttime hypoglycemia can cause sweating, shakiness, and abrupt awakenings that can blend into scary dreams for some people. If you’re on insulin or sulfonylureas and you’re having night sweats + nightmares, ask your clinician about checking overnight glucose patterns.
- GERD/reflux: reflux can trigger uncomfortable awakenings that make dreams feel more intense. If reflux is in the mix, avoid heavy/late meals, elevate the head of bed, and discuss persistent symptoms with a clinician.
- Chronic pain: pain can fragment sleep and increase stress arousals, which may worsen nightmares.
- Withdrawal from sedatives or sleep meds (including benzodiazepines): abrupt stopping can cause rebound insomnia, vivid dreams, and nightmares. If you’re tapering, do it with prescriber guidance.
What You Can Do Starting Tonight (No Crystal Required)
We’re going to break the nightmare-stress loop: nightmares wreck your sleep → you feel awful all day → you dread bedtime → you sleep less → nightmares get worse. It’s like a bad sitcom that won’t get canceled.
1) Get your sleep schedule boring on purpose
This is the least sexy fix—and one that helps many people. Pick a wake time you can stick to (yes, even weekends—temporarily) and build your bedtime around it.
Give it a couple weeks. Your brain likes routine the way toddlers like routine: it will fight you, then it may thrive.
2) Make your room a cave, not a runway
- Cool it down (many people sleep well in the mid-60s °F, but comfort varies)
- Kill random lights (LEDs, bright clocks, charger glow—why are they all so aggressive?)
- Put your phone far enough away that you can’t “just check one thing”
If you sleep next to a glowing rectangle, your brain stays in Scroll Mode. And Scroll Mode is not a restful spiritual state.
3) Do a short wind down that your nervous system understands
If you can’t do a two-hour spa routine, cool. Do 15-30 minutes of something genuinely calming: light reading, stretching, progressive muscle relaxation, slow breathing. The point is to send the message: “We’re safe. We’re done for the day.”
(And if you can swing it, yes: screens off earlier often helps—not because you lack willpower, but because bright, engaging content can keep your brain “on.”)
4) Empty your brain earlier in the evening
This is my favorite “I hate journaling but I hate nightmares more” trick: set a timer for 15 minutes at least a few hours before bed. Write down what’s stressing you and one tiny next action for each thing. When the timer ends, close the notebook.
Close it like you mean it. Boundaries, but make it stationery.
5) Track patterns in the morning (not at 3 AM)
In the morning, jot:
- what time it happened
- quick theme (chased, trapped, embarrassment, etc.)
- stress level the day before
- anything different: alcohol, meds timing, late coffee, bad sleep, illness
You’re not writing a memoir. You’re building a map.
Quick “What to Try First” Table (Nightly Nightmare Edition)
| Likely trigger | Clues it fits | What to try for 2-3 weeks | Evidence strength | Watch out for |
|—|—|—|—|—|
| Sleep deprivation / irregular schedule | short sleep, shifting bed/wake times | fixed wake time, protect total sleep time | Well established (sleep science) [AASM/SRS 2015] | don’t “catch up” with huge swings that worsen rhythm |
| Alcohol close to bedtime | nightmares later night, 3-5 AM wake ups | avoid alcohol within ~3-4 hours of bed | Promising/consistent sleep data [NIAAA] | withdrawal can worsen sleep—seek help if needed |
| Cannabis reduction/withdrawal | vivid dreams after cutting back | note timing of changes; stabilize routine | Mixed/individual [NCCIH] | talk to a clinician if you’re struggling to stop |
| Medication effect/timing | onset after med start/change | review timing with prescriber/pharmacist | Mixed; common in practice [Mayo Clinic] | don’t stop abruptly without guidance |
| Possible sleep apnea | snoring, witnessed apneas, daytime sleepiness | ask for OSA screening; consider sleep study | Well established for OSA; nightmare link varies [AASM: OSA] | untreated OSA has broader health risks |
| Trauma linked nightmares | replays, intense distress, avoidance | IRT + trauma focused therapy | Well established for IRT [Aurora 2010] | do therapy support if highly triggering |
What To Do When You Wake Up Terrified
When you wake from a nightmare, your body is basically yelling, “DANGER!” even though you are literally in pajamas. Your job is to talk your nervous system down.
- Breathing: inhale 4, hold 4, exhale 6 (do that 5-10 times). Longer exhale often feels more calming.
- Grounding: name 5 things you see, 4 you hear, 3 you can touch.
- Muscle relaxation: tense and release muscle groups from toes to face.
Try not to check the time. Don’t grab your phone (it’s basically choosing a jump-scare). If you’re still awake after ~20 minutes, get up briefly and do something boring in dim light until you feel sleepy again.
When It’s Time to Get Professional Help (Because Sometimes You Should Not DIY This)
Some nightmare seasons are a “tighten up your habits” situation. Some are a “please get support” situation. Here’s an easy way to sort it:
- Often OK to self-manage: less than ~1 nightmare/week and it’s not messing with your days.
- Schedule an evaluation: about 1+ per week for 3+ weeks, or it’s affecting mood, work, or sleep, or self-help hasn’t helped after 4-6 weeks.
- Don’t wait: near nightly nightmares, you’re avoiding sleep, or daytime functioning/safety is taking a hit.
- Urgent help now: suicidal thoughts, self-harm urges, or you’re acting out dreams and could get hurt.
Get urgent help now if you’re at immediate risk of harm.
- US: Call/text 988 (Suicide & Crisis Lifeline). Crisis Text Line: text HOME to 741741.
- Outside the US: contact your local emergency number or a country-specific crisis line (many regions list options via local health services).
Who do you even call?
- Primary care: possible sleep apnea, med related nightmares, illness/pain contributors, frequent nightmares.
- Sleep specialist: acting out dreams (possible RBD), suspected sleep apnea, unusual nighttime behaviors, injuries during sleep.
- Mental health professional: trauma linked nightmares, significant anxiety/depression, chronic nightmares despite the basics.
Getting the right help is not “being dramatic.” It’s being smart.
What to Expect at a Doctor Visit (So You’re Not Guessing)
If you book an appointment for nightmares every night, a clinician will typically:
- Take a sleep history (bed/wake times, awakenings, insomnia, snoring, naps)
- Review medications and substances (including timing, recent changes, alcohol/cannabis/nicotine, supplements)
- Ask about stress, anxiety, depression, and trauma symptoms (screening tools are common) [APA: PTSD overview]
- Screen for sleep apnea (questions + sometimes home sleep apnea testing or an in-lab study) [AASM: OSA overview]
- Consider polysomnography (sleep study) especially if there’s dream enactment/possible RBD, seizures, or complicated parasomnias [AASM: Parasomnias/RBD overview]
Helpful to bring: a simple 1-2 week log of nightmare timing, sleep schedule, caffeine/alcohol, and medication timing.
The Treatments That Actually Work (Not Just “Try Lavender”)
Lavender is lovely. Lavender is not a treatment plan.
Imagery Rehearsal Therapy (IRT)
This is a first line technique for recurring nightmares. You take the nightmare, rewrite the ending (or the scariest moment) so it turns safer, and rehearse the new version during the day [Aurora et al., 2010 (guideline)].
- Write the nightmare down (yes, in daylight).
- Pick the worst moment.
- Change one detail so it stops being terrifying.
- Rehearse the new version 15-20 minutes/day.
- Stick with it for 4-8 weeks.
If your nightmares are tied to trauma and feel extremely intense or graphic, consider doing this with a trauma trained therapist so you have support.
Prazosin (for PTSD related nightmares)
Prazosin is a blood pressure medication sometimes used to reduce PTSD related nightmares. Evidence is mixed: some studies show benefit, while others do not, so it’s a “shared decision” with your prescriber based on your symptoms and risk profile [VA/DoD PTSD CPG, 2023; Raskind et al., 2018 (clinical trial)].
Safety notes that matter:
- It can cause dizziness/lightheadedness and low blood pressure, especially when standing (orthostatic hypotension).
- Dosing and titration should be clinician led, particularly if you take other blood pressure meds.
Trauma focused therapy
If trauma is the driver, therapies like EMDR, Prolonged Exposure, or Cognitive Processing Therapy can reduce nightmares over time [APA: PTSD Treatments (overview); VA/DoD PTSD CPG, 2023]. It’s not about “reliving it for fun.” It’s about reclaiming your sleep and your life.
What I Want You to Do Next (Pick One)
If you’re overwhelmed, don’t try to overhaul your entire existence tonight. Pick one:
- Set a consistent wake time starting tomorrow.
- Move your phone away from the bed.
- Cut caffeine earlier for the next two weeks.
- Track nightmare timing for a week like a sleepy little detective.
- If you suspect meds or sleep apnea, make the appointment.
Better sleep isn’t a personality trait you’re missing. It’s usually a few toggles that need adjusting—sometimes with help, sometimes with simple changes you can start tonight.
Now go make bedtime boring in the best possible way.
Frequently Asked Questions
Why am I having nightmares every night all of a sudden?
A sudden nightly spike is often tied to a recent change: sleep loss, a new or adjusted medication, alcohol/cannabis changes, illness/fever, or a stress/mental health flare. Start by logging timing + recent changes for 1-2 weeks, and consider medical evaluation sooner if you also snore loudly, act out dreams, or feel unsafe.
Does anxiety cause nightmares?
Anxiety and stress can contribute to more frequent or more intense nightmares, especially when sleep is fragmented. The goal isn’t “never be stressed,” but to reduce the inputs that keep your nervous system on high alert: consistent sleep, a wind down routine, and targeted therapy if anxiety is persistent.
Can sleep apnea cause nightmares?
Sleep apnea can cause repeated arousals and drops in oxygen that fragment sleep; some people report distressing dreams or awakenings that feel like nightmares [AASM: OSA overview]. If nightmares come with loud snoring, witnessed breathing pauses, or major daytime sleepiness, ask about sleep apnea screening.
When should I do Imagery Rehearsal Therapy (IRT), and how long does it take?
IRT is typically practiced during the day, not at bedtime, for about 10-20 minutes daily. Many protocols suggest sticking with it for 4-8 weeks, and it has guideline support for recurrent nightmares [Aurora et al., 2010].
Are there risks to trying to “fix” nightmares on your own?
Basic sleep habits and tracking are generally low risk. Bigger risks include stopping medications abruptly, self-medicating with alcohol/sedatives, or doing trauma work alone if it becomes overwhelming—those are good reasons to involve a clinician.
Is melatonin or a supplement helpful for nightmares?
For nightmares specifically, evidence is stronger for behavioral treatments like IRT than for supplements. If you’re considering any supplement—especially if you’re pregnant, have a medical condition, or take other medications—check with a clinician or pharmacist first.
When should I see a doctor about nightmares?
See a healthcare provider if nightmares are weekly or more and impairing, if they persist beyond a few weeks despite sleep fixes, if you act out dreams, if you wake up gasping/choking, or if daytime sleepiness affects safety. Seek urgent help if you have suicidal thoughts, self-harm urges, or you’re at risk of harming yourself or someone else.
Sources
- American Academy of Sleep Medicine (AASM) Sleep Education. “Sleep Stages (NREM/REM) and Sleep Cycles.” https://sleepeducation.org/ (overview)
- Watson NF, Badr MS, Belenky G, et al. “Recommended Amount of Sleep for a Healthy Adult: A Joint Consensus Statement…” Sleep, 2015. (consensus statement)
- Aurora RN, Zak RS, Auerbach SH, et al. “Best Practice Guide for the Treatment of Nightmare Disorder in Adults.” Journal of Clinical Sleep Medicine, 2010. (guideline)
- American Academy of Sleep Medicine (AASM). Obstructive Sleep Apnea information/overview. https://aasm.org/ (overview)
- Mayo Clinic Staff. “Nightmares.” Mayo Clinic. https://www.mayoclinic.org/ (overview)
- Postuma RB, Iranzo A, Hu M, et al. “REM sleep behavior disorder and neurodegenerative disease risk…” The Lancet Neurology, 2019. (review)
- U.S. Department of Veterans Affairs / Department of Defense. “VA/DoD Clinical Practice Guideline for the Management of PTSD and Acute Stress Disorder.” 2023. (guideline)
- Raskind MA, Peterson K, Williams T, et al. “A Trial of Prazosin for Combat Trauma PTSD with Nightmares.” New England Journal of Medicine, 2018. (clinical trial)
- American Psychological Association (APA). “Clinical Practice Guideline / Treatments for PTSD.” https://www.apa.org/ (guideline/overview)
- National Institute on Alcohol Abuse and Alcoholism (NIAAA). “Alcohol and Sleep.” https://www.niaaa.nih.gov/ (overview)
- National Center for Complementary and Integrative Health (NCCIH). “Cannabis (Marijuana) and Cannabinoids.” https://www.nccih.nih.gov/ (overview)
- American Academy of Sleep Medicine (AASM). Parasomnias / REM Sleep Behavior Disorder overview. https://sleepeducation.org/ (overview)
- American Academy of Sleep Medicine. International Classification of Sleep Disorders, Third Edition (ICSD-3). 2014 (and subsequent text revisions). (classification reference)