Nightmares aren’t always “just a spooky little dream.” Sometimes they’re your brain flapping a tiny red flag in your face at 3 a.m. (which is honestly rude, but okay, message received).
There’s also research linking frequent nightmares with higher mental health risk, including suicidal thoughts and behaviors so if you’ve been brushing off bad dreams because you feel like you should be able to shake it off… you don’t have to white knuckle this [Nadorff et al., 2011; Pigeon et al., 2012].
The short answer: If nightmares are recurring and they’re affecting your daytime mood, safety, or functioning, it’s worth talking to a clinician (and sooner if there are red flags).
Key exception: If nightmares come with dream enactment (kicking/punching), breathing/choking symptoms, or thoughts of self-harm, don’t wait—seek urgent evaluation.
When it matters less: An occasional nightmare that doesn’t linger into your day is common, especially during stress—annoying, but not automatically “something serious.”
Quick triage: red flags (when to get help today vs soon)
Get help immediately (today):
- You have thoughts of self-harm or suicide, or you feel you might act on them. In the U.S., call/text 988. If you’re outside the U.S., contact your local emergency number or use findahelpline.com.
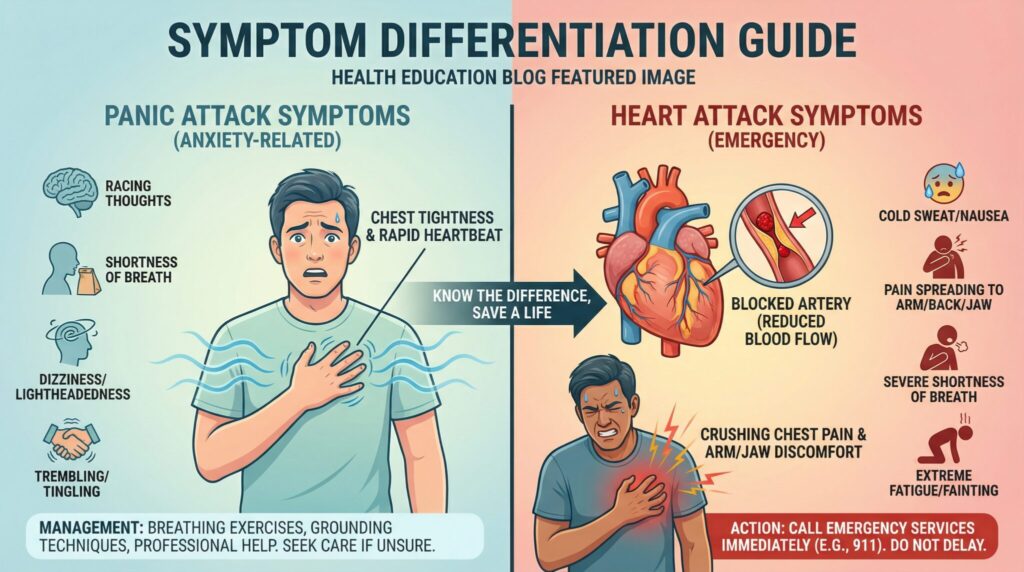
- You’re waking up gasping/choking, having chest pain, fainting, or severe shortness of breath.
- You’re acting out dreams (punching, kicking, falling out of bed) and someone could get hurt.
Get checked urgently (within days to 1-2 weeks):
- Nightmares are escalating fast, you’re avoiding sleep, or daytime sleepiness is affecting driving/work safety.
- Nightmares started after a medication change or substance withdrawal, and you feel unwell or unstable.
- New dream enactment symptoms, especially in older adults.
Bring it up at a routine appointment (but don’t ignore it):
- Recurring nightmares with daytime distress, anxiety, low mood, or worsening focus/energy.
- Nightmares that clearly track with stress/trauma and aren’t improving.
First: when is a nightmare actually a problem?
I’m not here to diagnose you over the internet (and frankly, I don’t want that kind of responsibility). But I can help you decide when it’s time to get checked out.
A nightmare crosses into “this deserves attention” territory when it’s not just scary—it’s messing with your life.
Clinically, nightmare problems are usually framed around recurrent nightmares + waking distress/impairment (for example: fear of sleep, fatigue, mood changes, or avoidance) rather than “the dream was intense” [DSM-5-TR; ICSD-3].
Not the vibe. Not the plot. Not whether there was a clown in the hallway (again). The real question is:
Are you paying for it during the day?
If your sleep is supposed to recharge you like a phone, nightmares are that background app draining your battery while pretending it’s not even open.
Daytime fallout is the receipt.
The usual suspects: why nightmares happen in the first place
Nightmares rarely pop up out of nowhere like a surprise party you didn’t ask for. They usually come with little sidekicks:
1) Stress and trauma
If you’ve been through something scary, upsetting, or ongoing (hello, chronic stress), nightmares can show up as your brain’s extremely unhelpful processing method.
And if you’re reliving the same scene over and over—especially if it’s tied to a real event—that’s a big clue that a trauma informed therapist could help. (PTSD related nightmares are common and treatable, but they can be stubborn without targeted care.)
2) Medication changes
Some medications are associated with more vivid dreams or nightmares, and for some people this shows up after starting, stopping, or changing a dose—though effects vary a lot by person and by medication [Wichniak et al., 2017; Warrington & Bostwick, 2006]. Examples that can be involved include:
- SSRIs/SNRIs (antidepressants)
- beta blockers
- corticosteroids
- stimulants
- nicotine replacement in some people (yes, really)
Important note: Do not stop a prescribed medication on your own because you think it’s causing nightmares. Call your prescriber. They can review risks/benefits and adjust dose/timing or switch you safely.
3) Alcohol/substances (including withdrawal)
Alcohol can disrupt sleep architecture, and withdrawal can cause REM “rebound” with unusually vivid dreaming for some people [Ebrahim et al., 2013]. If nightmares track with drinking or substance changes, that’s worth discussing honestly with a clinician—especially if you’re trying to cut back and feel physically off.
4) Sleep disruption, including sleep apnea
This one surprises people. Sleep apnea doesn’t always look like a cartoon snore. It can show up as:
- gasping/choking at night
- sweating, heart pounding
- very vivid “I’m drowning / I can’t breathe” dreams for some people
- daytime exhaustion even if you “slept 8 hours”
Treating sleep apnea may reduce nightmares in some people—especially when nightmares are tied to repeated awakenings and oxygen drops—but it’s not a guarantee and depends on the underlying cause [AASM OSA overview; Krakow et al., 2001].
A quick “look alikes” guide (because not everything scary at night is a nightmare)
Sometimes the nightmare is the headline. Sometimes it’s a clue that something else is going on.
| What it looks like | Possible “look alike” | Extra clues | Who to start with |
|—|—|—|—|
| You wake up terrified with a pounding heart, feel “impending doom” | Nocturnal panic | Often no clear dream story; can mimic a heart issue | Primary care + mental health clinician |
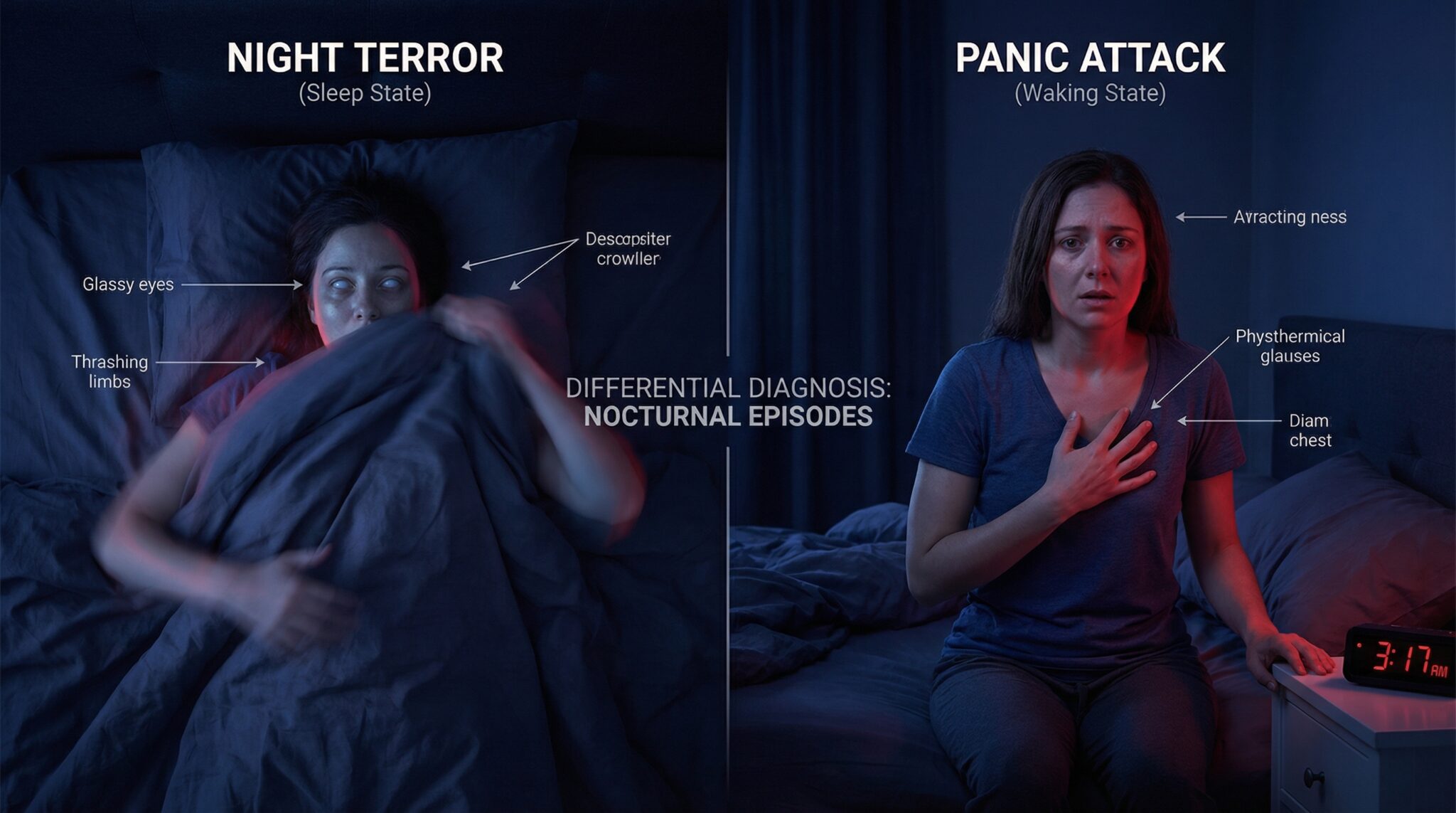
| You sit up, scream, thrash; hard to wake; little/no memory | Night terrors (NREM parasomnia) | More common in kids; often early in the night | Pediatrician/primary care; sleep specialist if frequent/injurious |
| You kick/punch/run, shout, fall out of bed | REM Sleep Behavior Disorder (RBD) | Dream enactment + injury risk; more common with age | Sleep specialist (sleep study often needed) [ICSD-3; Postuma et al., 2019] |
| Waking with burning throat, coughing, choking | GERD/laryngospasm | Worse after late meals, alcohol, certain foods | Primary care (and sometimes GI) |
| Confusion, tongue biting, bedwetting, injuries, odd repetitive movements | Nocturnal seizures | Often no dream recall; may have daytime spells too | Primary care urgently; neurology |
| “Vivid dreams + daytime sleep attacks” | Narcolepsy | Excessive daytime sleepiness, cataplexy, sleep paralysis | Sleep specialist |
If you’re not sure which lane you’re in, that’s okay. The point is: you don’t have to self-diagnose—you just want to start in the right neighborhood.
My “four week rule” (aka: when to stop toughing it out)
A simple benchmark that’s actually useful (and not a diagnostic cutoff):
If you’re having recurring nightmares (for example, about weekly) for several weeks and you’re dealing with daytime fallout, it’s time to talk to a clinician if you need ways to stop repeat nightmares.
Here’s a quick, honest checklist. No performing. Just facts.
It’s worth getting evaluated if you’re noticing things like:
- nightmares that keep happening (especially if they’re increasing)
- waking up from them regularly
- dreading bedtime (or procrastinating sleep like it’s taxes)
- worse mood, focus, or energy during the day
- avoiding activities/work/school because you’re wiped out
- nightmares started after a medication change, illness, or a traumatic event
- a bed partner reports you’re moving a lot, yelling, flailing, punching, etc.
If you’re checking multiple boxes, you’re not “being dramatic.” You’re gathering data.
Physical red flags I don’t want you to ignore
Sometimes nightmares are the main issue. Sometimes they’re a neon sign pointing to scary dreams that signal danger.
If you’re gasping, choking, sweating, or waking with a racing heart…
That can point to sleep apnea (or another medical issue), not just “bad dreams.” Especially if you snore, have high blood pressure, or feel tired no matter how long you sleep [AASM OSA overview].
If you’re acting out dreams (kicking, punching, falling out of bed)…
That’s a big one. During REM sleep, the body typically has muscle “atonia” (a built-in movement off switch). If that protective system fails, it can be REM Sleep Behavior Disorder (RBD) [ICSD-3].
This deserves prompt evaluation because injury risk is real.
Also gently and without alarmism RBD can be associated with neurodegenerative conditions later in life, particularly in older adults. That doesn’t mean you have (or will develop) one, but it does mean “don’t ignore it” and “get assessed properly” [Postuma et al., 2019].
Extra-important edge case: If you’re an older adult and dream enactment is new, or you have new tremor, stiffness, balance issues, or cognitive changes, seek evaluation sooner rather than later.
If nightmares come with thoughts of self-harm
This is an immediate, no-wait situation.
If you’re having suicidal thoughts, call/text 988 in the U.S. If you’re outside the U.S., contact your local emergency number or use findahelpline.com for country-specific crisis lines. If you’re in immediate danger, go to the nearest emergency department.
Okay, so who do you call?
If you’re staring at your phone like, “Primary care? Therapist? Sleep clinic?”—here’s the simplest roadmap:
- Start with your primary care clinician if you’re not sure. They can review meds, screen for common medical causes, and refer you out.
- See a sleep specialist if you suspect sleep apnea (snoring, breathing pauses, gasping) or dream enactment (possible RBD). A sleep study is commonly used when breathing disorders or parasomnias are suspected—not just “because nightmares,” but because of the pattern around them.
- See a mental health professional if nightmares are tied to trauma, anxiety, depression, or repeat themes that won’t quit.
And yes—there are treatments that genuinely help. One of the best supported options for recurring nightmares is Imagery Rehearsal Therapy (IRT), where you rewrite the nightmare while awake and rehearse the new version so your brain stops running the same horror clip on loop [Augedal et al., 2013; Krakow et al., 2001].
“Is this a nightmare or a night terror?” (because people mix these up constantly)
Nightmares and night terrors are not the same creature.
Nightmares:
- usually happen later in the night/early morning (often during REM)
- you wake up pretty alert
- you can often recall the dream in detail
- you want comfort (and water, and a new brain)
Night terrors:
- often happen in the first part of the night
- the person may scream/thrash but be hard to wake
- they usually don’t remember it the next day
- more common in kids [ICSD-3]
If you wake up fully alert with a clear memory of what happened in the dream, that points more toward nightmares.
How to prep for an appointment (so you don’t forget everything and panic talk)
Going to a sleep/medical appointment without notes is like going to Target without a list. You’ll walk out with a candle and no answers.
Do this instead:
For two weeks, jot down:
- bedtime and wake time
- nightmare nights (and whether you woke up)
- how long it took to fall back asleep
- caffeine/alcohol timing
- medication timing (including as needed meds)
- how you felt the next day (tired, anxious, fine-ish, etc.)
Also bring:
- a full med/supplement list (including cannabis/CBD if relevant)
- major stressors or recent life events
- anything your bed partner has noticed (snoring, gasping, movement)
Edge case to mention up front: If you have a history of seizures/epilepsy, fainting, significant heart disease, or you’re pregnant/postpartum and symptoms are escalating quickly, say so early in the visit—those details can change how urgently clinicians investigate nighttime events.
If you’re a parent reading this: kids and nightmares are their own thing
Seeing your kid scared at night hits different.
The good news: nightmares are common in kids, and many grow out of them as their brain and sleep patterns mature [AASM Parasomnias overview].
Consider professional help if:
- nightmares are frequent and persistent (for example, happening regularly for months)
- bedtime fear is intense or escalating
- your child is avoiding sleep or waking repeatedly and can’t settle back
- school, mood, behavior, or friendships are taking a hit
- the content includes sexual themes, extreme violence, or any disclosure that raises concern for abuse (that needs immediate attention)
Child adapted versions of IRT and anxiety/trauma focused therapies can be very effective, and a pediatrician can help you choose the next right step.
Frequently Asked Questions
When should I see a doctor about nightmares?
Consider it when nightmares are recurrent and you’re seeing daytime consequences—sleep avoidance, worsening mood, impaired concentration, or safety issues. Seek urgent care sooner if there’s dream enactment (kicking/punching), breathing symptoms (gasping/choking), or any self-harm thoughts.
Are frequent nightmares a mental health red flag?
They can be, especially when paired with anxiety, depression, PTSD symptoms, or suicidal thoughts. Research has found associations between nightmares and suicidality even after accounting for other factors, which is one reason clinicians take persistent nightmares seriously [Nadorff et al., 2011; Pigeon et al., 2012].
How often is “too often” for nightmares?
There’s no single magic number, but “too often” usually means they’re recurrent enough to cause distress or impairment (fear of sleep, fatigue, mood changes, functioning problems) [DSM-5-TR; ICSD-3]. If you’re noticing a pattern over several weeks, that’s plenty of reason to bring it up.
What’s the best treatment for recurring nightmares?
For many people, Imagery Rehearsal Therapy (IRT) is a strong first line, non-medication option with supportive evidence, including meta-analytic data [Augedal et al., 2013]. If nightmares are trauma related, trauma focused therapy may be recommended. Medication changes can also help when nightmares are medication or withdrawal related.
Can medications cause nightmares—and what should I do if I suspect that?
Some medications are linked to vivid dreams/nightmares in reviews and clinical experience, but it varies widely [Wichniak et al., 2017]. Don’t stop prescriptions abruptly—contact your prescriber to review timing, dose, interactions, and alternatives (especially with antidepressants, steroids, and stimulants).
Is “food/sleep hygiene” enough to stop nightmares?
Sometimes reducing sleep deprivation, alcohol, and stress helps—but persistent nightmares often need targeted treatment (like IRT) or evaluation for sleep disorders (like sleep apnea or RBD). If you’re doing the basics and still getting hit with nightmares + daytime fallout, that’s a good cue to level up to professional help.
When is it an emergency?
Get immediate help if you have suicidal thoughts, feel unsafe, or you’re acting out dreams with injury risk. Also seek urgent evaluation if you wake up gasping/choking, have chest pain, or daytime sleepiness is affecting driving or work safety.
The bottom line (because you don’t need a 47 step plan)
Nightmares become a “get help” issue when they affect your waking life—your mood, energy, focus, relationships, work, or your willingness to go to sleep at all.
And if you’re having trouble breathing at night, acting out dreams, getting injured, or having thoughts of self-harm? That’s not a “someday” problem. That’s a “today” problem.
You’re not weak for needing support. You’re not overreacting. You’re just tired—and your sleep is supposed to help with that, not ruin your mornings.
Go get your rest back. You deserve boring, peaceful sleep like it’s your birthright.
Sources
- American Academy of Sleep Medicine (AASM). Obstructive Sleep Apnea (OSA): overview and symptoms. https://aasm.org/resources/factsheets/sleepapnea.pdf (overview)
- American Academy of Sleep Medicine. International Classification of Sleep Disorders (ICSD-3). AASM, 2014. (diagnostic classification)
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM-5-TR). APA Publishing, 2022. (diagnostic criteria)
- Nadorff MR, Nazem S, Fiske A. “Insomnia symptoms, nightmares, and suicidal ideation in a college student sample.” Sleep, 2011. (observational study)
- Pigeon WR, Pinquart M, Conner K. “Meta-analysis of sleep disturbance and suicidal thoughts and behaviors.” Journal of Clinical Psychiatry, 2012. (meta-analysis)
- Augedal AW, Hansen KS, Kronhaug CR, Harvey AG, Pallesen S. “Randomized controlled trials of psychological and pharmacological treatments for nightmares: a meta-analysis.” Sleep Medicine Reviews, 2013. (meta-analysis)
- Krakow B, et al. “Imagery rehearsal therapy for chronic nightmares in sexual assault survivors with PTSD.” JAMA, 2001. (clinical trial)
- Wichniak A, Wierzbicka A, Jernajczyk W. “Effects of antidepressants on sleep.” Current Psychiatry Reports, 2017. (review)
- Warrington TP, Bostwick JM. “Psychiatric adverse effects of corticosteroids.” Mayo Clinic Proceedings, 2006. (review)
- Ebrahim IO, Shapiro CM, Williams AJ, Fenwick PB. “Alcohol and sleep I: effects on normal sleep.” Alcoholism: Clinical and Experimental Research, 2013. (review)
- Postuma RB, et al. “REM sleep behavior disorder and neurodegeneration—an update.” Sleep Medicine, 2019. (review)
- Find A Helpline. International crisis hotline directory. https://findahelpline.com (resource directory)