Every night, millions of people snore, but not all snoring is created equal. That rumbling sound might be perfectly harmless, or it could indicate something more serious that deserves attention.
Understanding snoring vs apnea can be confusing, which is why this guide breaks down everything you need to know.
You’ll learn the key differences between the two conditions, discover the warning signs that matter most, explore what the latest research reveals about diagnosis, and understand your treatment options.
By the end, you’ll have clarity on when to seek help and when you can rest easy.
What is Snoring?
Understanding the causes of snoring is essential for determining whether your nighttime breathing patterns warrant medical attention or simple lifestyle adjustments.
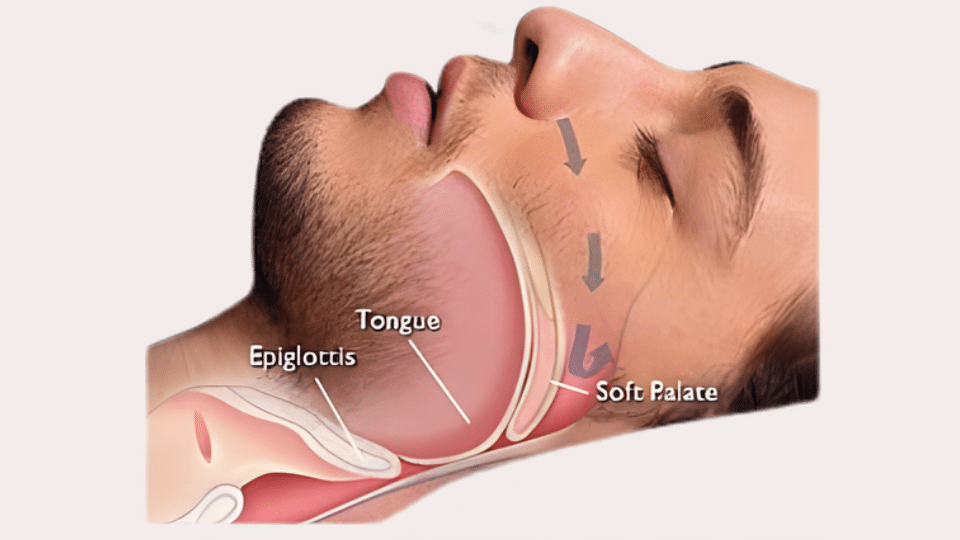
- Airflow obstruction: Narrowed airways force air through restricted passages, causing throat tissues to vibrate and create the characteristic rumbling sound
- Temporary factors: Nasal congestion, seasonal allergies, alcohol consumption before bed, and sleeping on your back can all trigger occasional snoring
- Weight-related issues: Excess weight, particularly around the neck, can put pressure on airways and increase snoring frequency
- Anatomical factors: A thickened soft palate, enlarged tonsils, or deviated septum can structurally narrow the airway
- The critical distinction: Occasional snoring after congestion or drinking is typically harmless, but frequent, loud snoring accompanied by breathing pauses may signal sleep apnea
Pay attention to patterns and accompanying symptoms, as distinguishing between harmless snoring and sleep apnea is crucial for your long-term health.
What is Sleep Apnea?
Sleep apnea is far more serious than simple snoring, involving repeated breathing interruptions that can significantly impact your health and sleep quality.
- A serious sleep disorder: Sleep apnea causes breathing to repeatedly stop and start throughout the night, disrupting normal sleep patterns
- Obstructive Sleep Apnea (OSA): The most common form occurs when throat muscles relax excessively, causing the airway to collapse or become completely blocked
- Breathing pauses: These interruptions can last 10 seconds or longer, representing complete or partial airway obstruction rather than simple tissue vibration
- Oxygen deprivation: Each pause triggers a dangerous drop in blood oxygen levels, forcing the body into a stress response
- Sleep disruption cycle: The brain must briefly rouse from sleep to reopen the airway, sometimes dozens of times per hour without full awakening
- Poor sleep quality: Despite spending adequate hours in bed, the constant interruptions result in fragmented, non-restorative sleep
This cycle of oxygen drops and sleep fragmentation explains why untreated sleep apnea leads to daytime exhaustion and serious health complications.
Key Differences between Snoring and Sleep Apnea
While both conditions involve nighttime breathing issues, the snoring vs apnea distinction comes down to what’s actually happening in the airway, and the health consequences.
| Feature | Snoring | Sleep Apnea |
|---|---|---|
| What’s Happening | Airway vibration creates noise | Airway collapses, blocking breathing |
| Breathing Pattern | Continuous (though noisy) | Repeated pauses or shallow breaths |
| Nighttime Symptoms | Sound, occasional tossing | Gasping, choking, frequent awakenings |
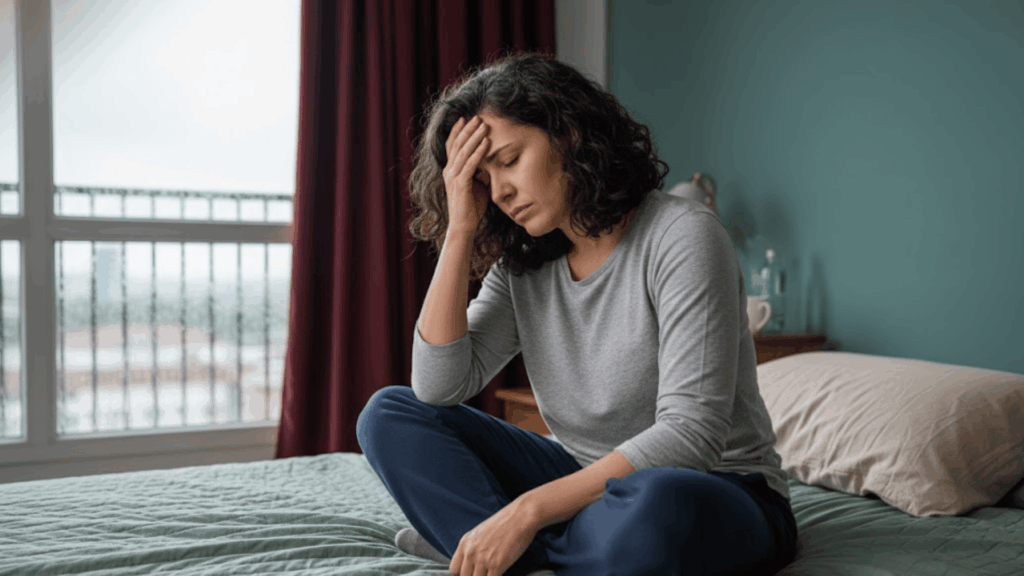
| Morning/Daytime Effects | Minimal to none | Exhaustion, headaches, irritability, brain fog |
| Health Risks | Generally low | Elevated risk for heart disease, diabetes, hypertension, stroke |
It is important to know that not all snorers have sleep apnea, and some people with apnea snore quietly or not at all. Symptoms beyond sound matter most.
How to Tell if It’s Sleep Apnea
Determining the difference between snoring vs apnea requires both observation and medical evaluation. Here’s what to watch for and when to seek professional help.
- Ask a sleep partner or roommate: They’re often first to spot breathing pauses, gasping, or choking sounds that distinguish apnea from simple snoring
- Monitor daytime warning signs: Excessive fatigue despite adequate sleep hours, persistent morning headaches, difficulty concentrating, or unexplained high blood pressure
- Consider medical evaluation: Sleep specialists use in-lab or home sleep studies to measure breathing patterns, oxygen levels, and sleep disruptions with precision
- Find out with additional testing: Clinical questionnaires and ENT examinations can identify anatomical issues or rule out other conditions
If symptoms extend beyond nighttime noise, professional assessment is the safest path to accurate diagnosis and effective treatment.
Health Risks of Untreated Sleep Apnea
Unlike simple snoring, untreated sleep apnea carries serious health consequences. The repeated oxygen drops and sleep disruptions take a cumulative toll on the body.
In the short term, expect poor-quality sleep that leads to excessive daytime drowsiness, difficulty concentrating, memory problems, mood swings, irritability, and depression.
The long-term risks are more alarming. Chronic sleep apnea significantly increases the risk of hypertension, heart disease, stroke, and type 2 diabetes.
The constant stress on the cardiovascular system from oxygen deprivation doesn’t just affect sleep; it affects lifespan. Additionally, severe daytime fatigue raises the risk of workplace accidents and drowsy driving incidents.
One Week Routine for Snoring and Sleep Apnea Management
This one week routine turns proven snoring and sleep apnea treatments into simple, daily actions you can follow consistently.
| Day | Morning | Afternoon | Evening |
|---|---|---|---|
| Day 1 | Record baseline symptoms and weight | Schedule therapy, gather supplies | Avoid alcohol, nasal rinse, side sleeping |
| Day 2 | Check CPAP or appliance fit, clean equipment | Light exercise, hydrate well | No alcohol or sedatives, nasal care, side sleeping |
| Day 3 | Assess sleep quality and alertness | Avoid late caffeine, practice nasal breathing | Jaw or throat exercises, consistent bedtime |
| Day 4 | Review snoring feedback or device data | Optimize sleep environment | Side sleeping, light dinner |
| Day 5 | Reassess energy and weight | Moderate exercise, limit screens | Nasal care, full night therapy use |
| Day 6 | Identify comfort issues and adjust | Reduce evening salt, hydrate | Early bedtime, strict alcohol avoidance |
| Day 7 | Compare symptoms to Day 1 | Plan next steps or follow up | Maintain full routine |
Improvement comes with consistency; persistent symptoms mean professional evaluation and long term treatment are needed.
What Research Says About Snoring and Sleep Apnea
A 2019 study published in the Journal of Clinical Sleep Medicine challenges common assumptions about the snoring vs apnea connection.
Researchers at Toronto Rehabilitation Institute analyzed 235 patients using machine learning to measure snoring frequency objectively.
Many people without sleep apnea snored just as frequently as those with severe cases. Snoring showed high sensitivity (91%) but very low specificity (31%), meaning frequent snorers often had no apnea at all.
The researchers concluded that snoring frequency alone offers “limited usefulness” in determining sleep apnea presence or severity, reinforcing why professional sleep studies remain essential for accurate diagnosis.
The Bottom Line
Now you have a clearer picture of what separates harmless snoring from sleep apnea. The key takeaway? Not all snoring requires medical intervention, but certain warning signs, such as breathing pauses, chronic fatigue, and morning headaches, shouldn’t be ignored.
If you’re experiencing symptoms beyond simple noise, a sleep study can provide definitive answers. And if it turns out you do have sleep apnea, effective treatments exist that can dramatically improve your sleep quality and overall health.
The difference between snoring and apnea might seem subtle, but addressing the right one makes all the difference in how you feel every day.
Looking for more sleep health insights? Read our related articles on improving sleep quality.