There are few things more rude than waking up at 3:00 AM absolutely convinced your heart is trying to break out of your ribcage and start a new life as a percussion instrument.
And here’s the annoying part: it can feel super dramatic…and still be caused by something boring like caffeine, alcohol, dehydration, stress, or the fact that you’re sleeping folded up like a dropped pretzel.
The short answer: Nighttime heart racing/palpitations are often triggered by sleep disruption, stimulants (caffeine/nicotine), alcohol, dehydration, reflux, stress, or medications but persistent, new, or symptomatic episodes deserve medical evaluation.
Key exception: If you have chest pain, fainting, severe shortness of breath, or a sustained very fast/irregular rhythm, treat it as urgent.
When it matters less: If it’s brief, infrequent, and clearly tied to a trigger (late caffeine, alcohol, stress), a simple “one change at a time” experiment often helps.
Also: I’m not your doctor. I’m just a person who likes practical checklists and hates 3 AM spirals. Use this as info, not a diagnosis.
First: why it feels SO loud at night
Your heart isn’t necessarily doing anything brand new at night you’re just finally noticing it.
During the day, your brain is busy doing daytime brain things (work, errands, doomscrolling, remembering you left laundry in the washer again). At night it’s quiet, you’re still, and suddenly your heartbeat is the only show in town. So every thump feels amplified like turning the volume up on background noise you didn’t realize was there.
A few real physical things can also make nighttime palpitations feel more intense:
- Your sleep position can change what you feel. A lot of people notice it more on their left side (your heart is closer to the chest wall), and some people feel weird on their back too.
- When you lie down, blood shifts around. More blood returns toward your chest compared to standing up, and sometimes that makes your heartbeat feel “bigger.”
- Early morning hormones do their thing. Your body starts nudging itself toward waking up in the early morning hours, and that can come with a small heart rate bump (part of normal circadian biology) [AHA: Palpitations overview].
So yes: sometimes nothing is “wrong,” it’s just your body existing loudly in the dark. Deeply unhelpful. But often normal.
Quick self-check: “palpitations” vs a truly fast or irregular rhythm
“Palpitations” can mean a lot of things: pounding, fluttering, skipped beats, or a fast rate. Two quick checks can make your next step clearer (and make a clinician visit way more useful).
1) Check your pulse (the simple way)
- Use two fingers on the thumb side of your wrist (radial pulse), or the side of your neck (carotid pulse only don’t massage).
- Count beats for 30 seconds and double it.
- Resting heart rate over ~100 bpm is generally considered tachycardia (fast rate) [NHS: Palpitations, Mayo Clinic: Tachycardia].
2) Check the pattern: regular or irregular?
- Regular fast (like a steady drumbeat) can happen with anxiety, caffeine, dehydration, fever, or sometimes a rhythm like SVT.
- Irregular (unpredictable spacing) is more likely to reflect premature beats (very common) or an arrhythmia that should be evaluated especially if it’s new or you feel unwell [AHA: Arrhythmia/palpitations overview].
Smartwatch note: wearables can be helpful for trends, but false alarms happen especially with movement, poor skin contact, or anxiety spirals. Use it as a clue, not a verdict [AHA: Wearables and heart rhythm].
The usual suspects (aka: check your pantry before you panic)
If your heart does this at night, I’d start here because these are common, fixable, and honestly kind of sneaky.
1) Caffeine (including the “I barely had any!” kind)
Caffeine can hang around longer than it has any right to. Even if you fall asleep fine, it can still stir things up later especially in people who metabolize it more slowly [FDA: Caffeine basics].
Hidden-ish sources:
- afternoon coffee/tea (obviously)
- “decaf” (it’s not caffeine-free, it’s just less guilty)
- chocolate
- pre-workout/energy drinks
- some cold/flu meds (look for stimulant decongestants like pseudoephedrine)
Try this: cut caffeine after noon for 3 days. If your night heart drama improves, congratulations/condolences you found a trigger.
If you’re on stimulants (ADHD meds), thyroid medication, or inhalers: don’t stop prescribed meds on your own but do mention nighttime palpitations to the prescriber, because dose/timing tweaks can matter [NHS: Palpitations causes].
2) Alcohol (the sleep liar)
Alcohol can make you sleepy at first…then fragment sleep later. In some people, it can also raise heart rate and trigger palpitations/arrhythmias (including “holiday heart” patterns) [AHA: Alcohol and heart rhythm, Voskoboinik et al., 2020].
Try this: finish any alcohol earlier in the evening (like by dinner) for a week and see what changes.
3) Dehydration + heavy late night eating
If you’re low on fluids, your heart may compensate with a faster rate. And if you eat a big, salty/sugary/fatty meal close to bedtime, your body is doing digestion gymnastics when it should be powering down.
Quick reality check: if your urine is dark yellow, you may need more fluids. (Not glamorous, but effective.)
If you have kidney disease or heart failure: fluid targets can be different follow your clinician’s guidance rather than pushing extra fluids.
4) The anxiety ↔ palpitations doom loop
This one is so common it deserves a little spotlight.
You notice your heart.
You think, “Uh oh.”
Your body goes, “UH OH INDEED,” and releases stress hormones.
Your heart beats faster.
You notice it more.
And now you’re fully awake doing mental math about your pulse and your mortality.
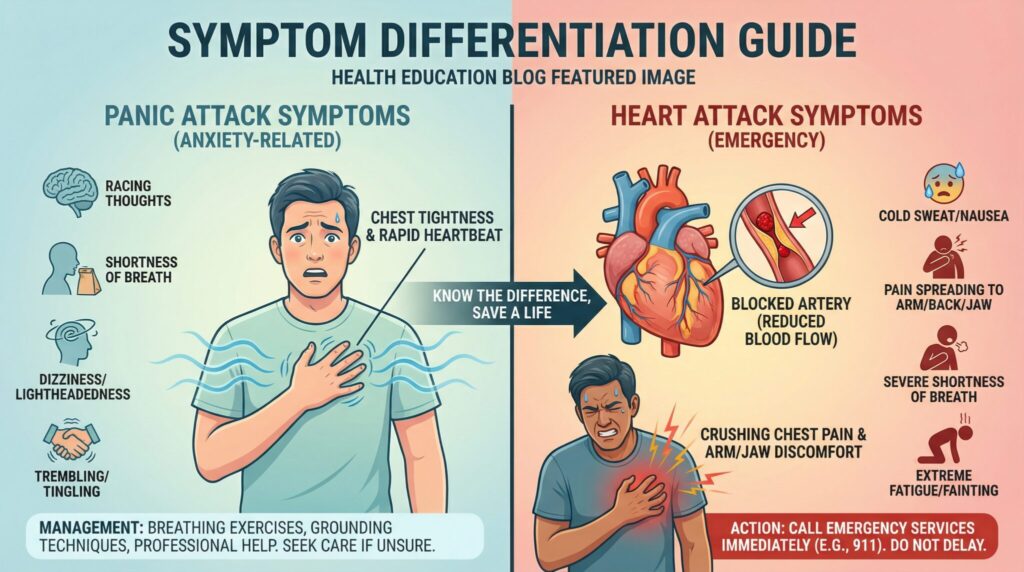
If it’s anxiety driven, slow breathing can help within a minute or two by nudging your nervous system toward “stand down” mode [Harvard Health: Relaxation response overview]. True rhythm issues can sometimes keep going no matter how zen you’re trying to be so don’t use breathing as a perfect test, but it’s a clue.
Other common causes people miss (the “Google expects this” list)
These are common enough and important enough that they deserve a spot on your checklist:
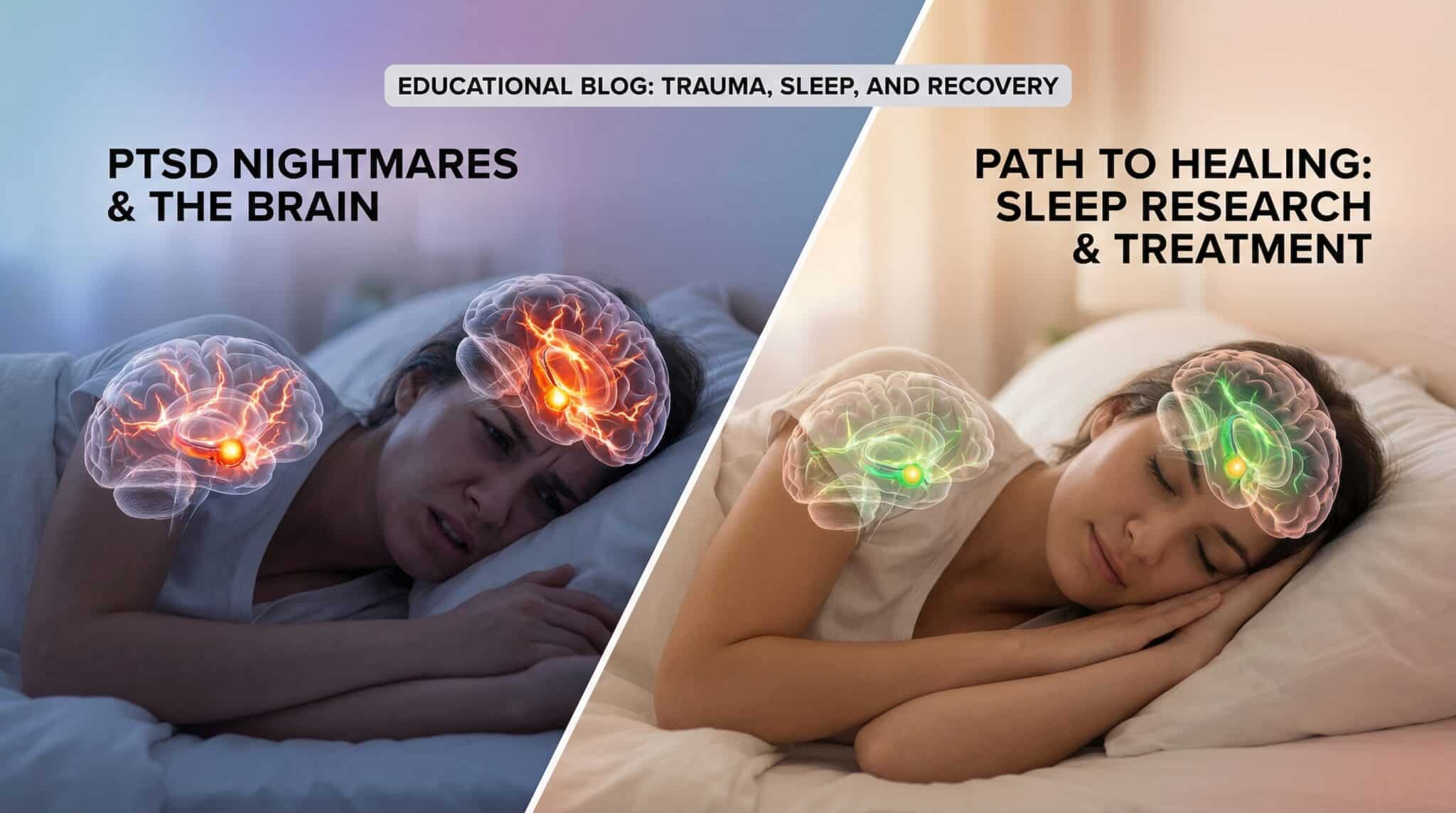
- Obstructive sleep apnea (OSA): If you snore, gasp/choke awake, have morning headaches, or feel wiped out in the daytime, OSA can trigger nighttime surges in heart rate and palpitations [AASM: Sleep apnea overview, AHA: Sleep apnea and cardiovascular risk].
- GERD/reflux: Acid reflux can flare when you lie down and sometimes feels like chest fluttering or can trigger palpitations via discomfort/adrenaline. If palpitations show up with heartburn, sour taste, or a burning chest, reflux is worth addressing [NHS: Palpitations causes].
- Nicotine/cannabis: Nicotine is a stimulant. Cannabis can raise heart rate in some people either can worsen nighttime palpitations, especially with anxiety or higher doses [CDC: Tobacco health effects, NIDA: Cannabis effects].
- Fever/infection: Being sick (even “just a virus”) can push heart rate up, especially with fever or dehydration.
- Low blood sugar overnight: More common if you’re on insulin or diabetes meds, or you skip dinner and then wake sweaty/shaky with a racing heart.
- Hormonal shifts: Perimenopause/menopause hot flashes and night sweats can come with a pounding heart sensation. Pregnancy also increases heart workload and can change how palpitations feel [ACOG: Pregnancy physiologic changes].
- Thyroid issues, anemia, electrolyte imbalance: Overactive thyroid, low iron, or electrolyte changes can all contribute to palpitations and should be checked if symptoms persist or come with fatigue, tremor, weight change, or shortness of breath [Mayo Clinic: Palpitations causes].
- POTS/orthostatic intolerance: If the racing is mostly when you stand up (even at night to use the bathroom) and you get lightheaded, that pattern is worth bringing up.
Common triggers at a glance
| Possible trigger | Common clues | What to try first | When to get checked sooner |
|---|---|---|---|
| Caffeine / stimulants (incl. decongestants, pre-workout) | Worse after afternoon intake, jittery, trouble staying asleep | Cut after noon, review labels/meds | New symptoms after starting/changing meds |
| Alcohol | Wakes you in lighter sleep, sweating, pounding heart | Stop earlier, reduce/skip for a week | If you get irregular rhythm or shortness of breath |
| Dehydration | Dark urine, dry mouth, more after hot day/exercise | Hydrate earlier in day | If you’re on diuretics or have kidney/heart failure (ask clinician) |
| Big/late meal or reflux | Heartburn, sour taste, worse lying flat | Earlier/lighter dinner, elevate head | Chest pain that’s new/unclear → urgent evaluation |
| Anxiety/stress | “Uh oh” spiral, improves with slow breathing | Long exhales, grounding | If panic symptoms mimic heart symptoms and it’s new get assessed |
| Sleep apnea | Snoring, gasping, daytime sleepiness | Side sleeping, ask about sleep study | If you have high BP, obesity, or witnessed apneas |
| Fever/infection | Sick, fever, body aches | Fluids, treat fever per guidance | If chest pain, fainting, or severe shortness of breath |
| Hormones (peri/menopause, pregnancy) | Hot flashes/night sweats, pregnancy symptoms | Cooling strategies, prenatal care | Pregnancy + new/persistent palpitations → mention promptly |
| Thyroid/anemia/electrolytes | Tremor, weight change, fatigue, cramps | Don’t self-supplement aggressively | Persistent episodes → labs/ECG |
What to do in the moment (instead of spiraling)
When you wake up with your heart racing, your job is not to “figure out your entire life.” Your job is to do a few simple things in order and let your nervous system catch up.
Here’s what I’d try:
1) Change position
Roll onto your right side, or prop yourself up a bit (even a second pillow can help). Sometimes it’s really that simple especially if reflux or sleep position is part of the problem.
2) Do a slow breath reset (my go to)
Try 4-7-8 breathing:
- inhale 4
- hold 7
- exhale 8
Do 4-5 rounds.
If you hate counting (fair), just focus on longer exhales than inhales.
3) Consider a vagal maneuver (ONLY for a fast, regular rhythm and only if you feel otherwise okay)
Vagal maneuvers can sometimes slow certain rapid, regular rhythms (like SVT). A modified Valsalva technique has clinical trial support in emergency settings [Appelboam et al., 2015 (REVERT trial)].
Safer home version to try:
- Bear down like you’re trying to have a bowel movement for ~10-15 seconds, then relax.
Avoid:
- Carotid massage (do not do this at home).
- Any maneuver if you have chest pain, severe shortness of breath, fainting/near fainting, new weakness/numbness, or you simply feel “wrong.”
If this is your first severe episode, the rhythm is irregular, or it’s not settling down: skip DIY and get medical help.
4) Sip water
If dehydration is part of your issue, water can help. If you’re also sweaty/shaky and you’re at risk for low blood sugar (diabetes meds/insulin), check your glucose if you can and treat per your plan.
5) Get up briefly (calmly)
If you’re still keyed up, stand and walk slowly in dim light for a minute or two gentle movement, not frantic pacing.
How to prevent the 3 AM sequel
If you want the biggest bang for your effort, don’t overhaul your whole life. Run a simple “one change at a time” experiment (because if you change five things at once, you won’t know what helped).
If it were me, I’d do this in tiers:
Week 1: the big hitters
- No caffeine after noon
- Alcohol earlier (or skip it for a week if you’re up for a clean test)
- Hydrate during the day (not chugging a lake at 10 PM)
- Try not to eat a heavy meal right before bed
- If reflux is suspicious: earlier dinner, smaller/fattier foods dialed down, and consider head of bed elevation
Week 2: calm your nervous system on purpose
- Screens away 60 minutes before bed (I know, I know)
- Do 2 minutes of slow breathing before you fall asleep, not just during a panic moment
- Experiment with sleep position if you suspect it matters
- If snoring/gasping/daytime sleepiness is in the picture: ask about sleep apnea screening (it’s a big one) [AASM: Sleep apnea overview]
When to get help (this is the no-jokes part)
Many palpitations are benign. But some are not especially when they come with warning signs [AHA: Palpitations overview].
Call emergency services right away if you have:
- chest pain/pressure/tightness that lasts more than a few minutes
- fainting or feeling like you’re about to pass out
- severe shortness of breath that doesn’t improve when you sit up
- a very fast heart rate at rest that stays high and isn’t trending down after ~15-20 minutes of quiet rest, especially if you feel unwell [NHS: Palpitations]
- an obviously irregular rhythm plus dizziness, chest discomfort, or shortness of breath
- new neurologic symptoms (weakness, trouble speaking, facial droop)
If you’re reading that list thinking, “Wait…that’s me,” stop googling and get help.
Make a non-urgent appointment if:
- it’s happening more than a couple times a week
- episodes regularly last 5-15 minutes (or longer)
- it’s new for you (especially if you’re over 40)
- there’s no clear trigger (no caffeine, no alcohol, no stress spike…still happening)
- you have other health conditions (high blood pressure, diabetes, thyroid issues), you’re pregnant/postpartum, or you have a strong family history of rhythm problems or sudden cardiac death
If you do see a doctor, here’s what usually happens (so you’re not blindsided)
Most “palpitations workups” are pretty straightforward [Mayo Clinic: Palpitations diagnosis].
- ECG/EKG: quick snapshot of your heart rhythm (helpful, but it might look normal if you’re not having symptoms right then)
- Bloodwork: often checks thyroid, electrolytes, and anemia
- Monitor (Holter/event monitor): if your symptoms are intermittent, they may have you wear a monitor to catch what’s happening during a real episode
- Sleep evaluation: if sleep apnea signs are present (snoring, gasping, daytime sleepiness), a sleep study may be part of the plan [AASM: Sleep apnea overview]
Do yourself a favor: jot down a quick note for a week time it happened, how long it lasted, your pulse (if you checked), what you ate/drank, stress level, sleep position, and what helped. This turns your appointment from “vibes and fear” into actual usable clues.
Frequently Asked Questions
Why does my heart race when I lie down at night?
Often it’s a mix of “you notice it more” plus position related changes (like reflux, pressure on the chest, or normal blood flow shifts when you lie down). Alcohol, caffeine, and stress can also make lighter sleep more likely so you catch every thump.
Can sleep apnea cause nighttime palpitations?
Yes. Obstructive sleep apnea can cause repeated drops in oxygen and stress hormone surges that raise heart rate and can trigger palpitations during the night [AASM: Sleep apnea overview, AHA: Sleep apnea and cardiovascular risk]. If you snore loudly, gasp awake, or have significant daytime sleepiness, it’s worth discussing a sleep study.
How fast is “too fast” at night and how do I check?
A resting heart rate over ~100 bpm is generally considered tachycardia [NHS: Palpitations, Mayo Clinic: Tachycardia]. Check your pulse for 30 seconds and double it. Also note whether it feels regular or irregular.
Is it anxiety or an arrhythmia?
Anxiety can absolutely cause a fast, regular heartbeat and a “doom loop,” and slow breathing may help it settle. An arrhythmia is more likely if the rhythm feels irregular, episodes come out of nowhere without a trigger, you faint/near faint, or you have chest pain or significant shortness of breath [AHA: Palpitations overview].
Are vagal maneuvers safe to do at home?
They can be reasonable only if you’re otherwise well and the rhythm seems fast and regular (possible SVT). Avoid carotid massage, and stop/seek care if you have chest pain, severe shortness of breath, fainting/near fainting, or neurologic symptoms [Appelboam et al., 2015].
What if I have diabetes, reflux/GERD, or I’m pregnant?
If you’re monitoring blood sugar, nighttime racing with sweating/shaking can be hypoglycemia check glucose if possible and treat per your plan. If you have reflux, avoid late heavy meals/alcohol and consider head elevation. During pregnancy (or postpartum), new or persistent palpitations should be mentioned promptly because evaluation thresholds are often lower [ACOG: Pregnancy physiologic changes].
When should I see a doctor about sleep related heart racing?
See a clinician if it’s new, happening more than a couple times a week, lasting more than ~15 minutes, or affecting daytime functioning. Seek urgent care sooner if you have episodes with chest pain, fainting/near fainting, severe shortness of breath, sustained very fast heart rate at rest, or an irregular rhythm with symptoms [NHS: Palpitations, AHA: Palpitations overview].
The goal: boring sleep and a quiet heart
Nighttime heart racing is one of those things that feels terrifying and mysterious…until you realize it’s often triggered by very normal stuff. Start with the simplest experiments (caffeine cutoff, alcohol timing, hydration, late night meals), use the calming steps when it happens, and keep an eye out for the true red flags.
And tonight just pick one change to try. Not fifteen. One.
May your bedroom be dark, your brain be quiet, and your heartbeat be aggressively boring.
Sources
- American Heart Association (AHA). Palpitations/Arrhythmia patient overviews, Wearables and heart rhythm. https://www.heart.org/ (overview)
- National Health Service (NHS). “Heart palpitations.” https://www.nhs.uk/conditions/heart-palpitations/ (overview)
- Mayo Clinic. “Tachycardia” and “Heart palpitations” (causes/diagnosis). https://www.mayoclinic.org/ (overview)
- American Academy of Sleep Medicine (AASM). Obstructive sleep apnea overview. https://sleepeducation.org/sleep-disorders/obstructive-sleep-apnea/ (overview)
- U.S. Food & Drug Administration (FDA). “Spilling the Beans: How Much Caffeine is Too Much?” https://www.fda.gov/food/food-additives-petitions/spilling-beans-how-much-caffeine-too-much (overview)
- Appelboam A, Reuben A, Mann C, et al. “Postural modification to the standard Valsalva manoeuvre for emergency treatment of supraventricular tachycardias (REVERT).” The Lancet, 2015. (randomized clinical trial)
- Voskoboinik A, Kalman JM, De Silva A, et al. “Alcohol Abstinence in Drinkers with Atrial Fibrillation.” New England Journal of Medicine, 2020. (randomized clinical trial)
- American College of Obstetricians and Gynecologists (ACOG). Pregnancy physiologic changes/pregnancy care resources. https://www.acog.org/ (overview)
- Centers for Disease Control and Prevention (CDC). Health effects of tobacco/nicotine. https://www.cdc.gov/tobacco/ (overview)
- National Institute on Drug Abuse (NIDA). Cannabis drug facts (effects including heart rate). https://nida.nih.gov/publications/drugfacts/cannabis-marijuana (overview)
- Harvard Health Publishing. Relaxation response/slow breathing overview. https://www.health.harvard.edu/ (overview)