By: (Your Name / Site)
Last updated: 2025-12-23
Editorial note: This guide is for education and discussion with a qualified clinician. It’s not personal medical advice or a substitute for diagnosis or treatment.
If you have PTSD nightmares, you’re not “being dramatic.” You’re not “too sensitive.” Your brain is doing that deeply annoying thing where it tries to protect you… by replaying the scariest content it has on file. Over. And over. And over.
The short answer: PTSD nightmares are common, vivid, and often tied to ongoing hyperarousal. The best-supported targeted treatments are Image Rehearsal Therapy (IRT) and (for some people) prazosin, alongside trauma-focused care and sleep-disorder screening.
Key exception: If you’re waking up gasping/choking, acting out dreams, getting injured, or feeling unsafe (including suicidal thoughts), you need medical evaluation urgently, not just self-help.
When it matters less: If nightmares are occasional and not impairing your daytime life, you may not need intensive treatment basic sleep support and stress skills may be enough.
About 70% of people with PTSD report trauma-related nightmares, compared with roughly 2-8% of the general population experiencing frequent nightmares (definitions vary) [Germain, 2013. AASM ICSD-3]. So if your nights feel like your nervous system is running a high-budget horror series with surround sound and zero commercial breaks unfortunately common. Also: treatable.
I’m going to walk you through (1) why these nightmares feel so real, (2) what actually helps specifically prazosin and Image Rehearsal Therapy (IRT) and (3) what you can do tonight when you wake up with your heart doing parkour.
Why PTSD nightmares aren’t “normal nightmares with better special effects”
A regular nightmare tends to be… weird. Like, you’re late to a math test in a mall, your teeth fall out, and your boss is a dolphin. Classic dream nonsense.
PTSD nightmares often don’t do nonsense. They can be clear, linear, and disturbingly realisticsometimes replaying the trauma directly (“replicative” content), not just symbolizing it [Germain, 2013]. And your body can react like it’s happening right now: sweating, racing heart, that jolt of panic that doesn’t fade in 10 seconds.
It’s like your brain skipped the “this is just a dream” disclaimer and went straight to full sensory replay.
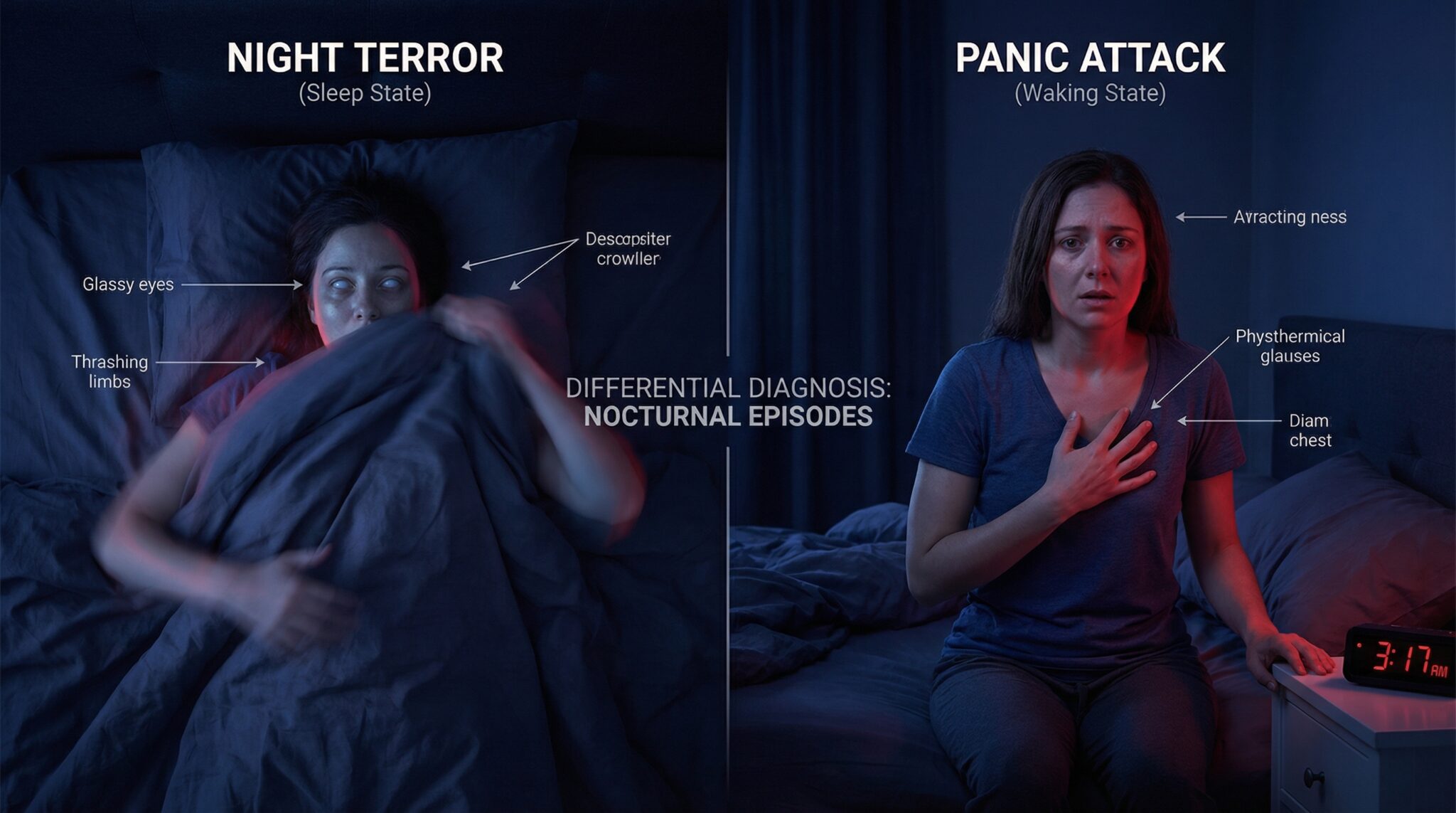
“Is this a night terror?”
Here’s a simple way to tell the difference:
- PTSD nightmares: you usually remember them. Vividly. Unfortunately.
- Night terrors: often come with little to no memorysomeone might tell you you were screaming or thrashing, and you’re like, “I was… asleep?” [AASM ICSD-3]
If you’re having violent sleep behavior, new night terrors in adulthood, or anything that could cause injury, that’s a “get checked out” situation if you need to tell night terrors apart because there are other sleep disorders (like REM sleep behavior disorder, seizures, or untreated sleep apnea) that deserve a proper medical workup [AASM ICSD-3].
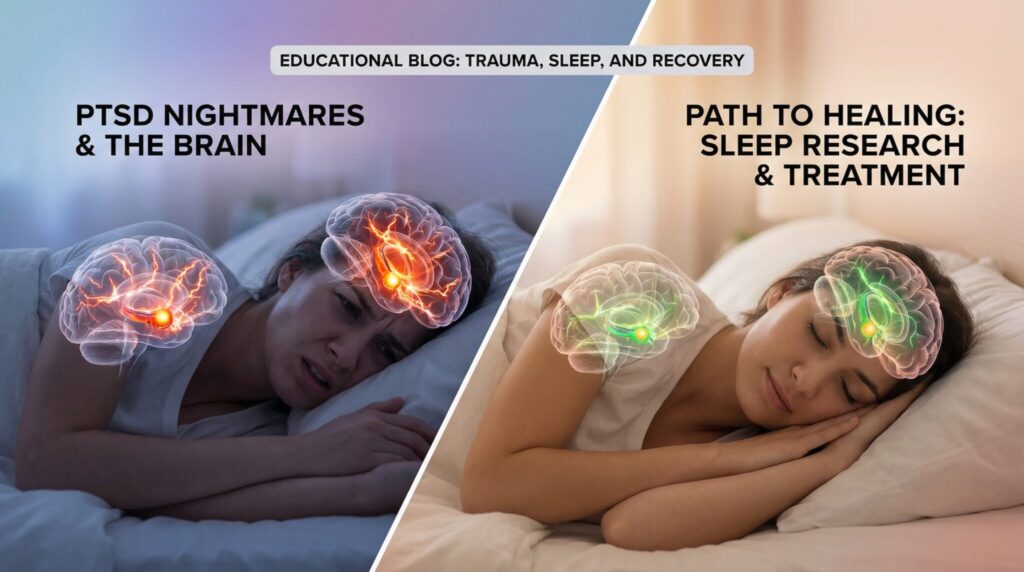
What your brain is doing wrong at night (and why it feels so real)
Here’s the most helpful way I’ve heard it explained: PTSD turns your internal smoke alarm into a smoke alarm that also screams “FIRE!” when you make toast.
In PTSD nightmares, systems involved in threat detection and memory processing may stay more “on” than we’d like during sleepespecially around REMso the dream can come with real physiological alarm [Germain, 2013]. Some researchers describe a “nightmare circuit,” but the simple translation is: your brain’s night shift is mismanaged.
A few key things can happen:
- Your threat system stays too “on.” (Think: amygdala = overachieving alarm.)
- Your memory system doesn’t file the trauma away cleanly. (Think: hippocampus = messy filing cabinet.)
- The “this isn’t real, it’s a dream” signal is weaker (less top-down braking).
- Stress chemistry can keep running at night, including norepinephrine, which is linked to hyperarousal and may intensify trauma dreams for some people [Germain, 2013. Raskind et al., 2007].
So you get the perfect storm:
- your body doesn’t fully downshift,
- scary memories get activated without enough “I’m safe now” context,
- and the nightmare can reinforce fear instead of softening it.
The good news (the science kind): the brain can change. Nightmare patterns can improve a lot with the right treatment [AASM Position Paper, 2018].
The cycle that keeps nightmares coming (aka: the world’s worst subscription service)
Nightmares disrupt sleep. Disrupted sleep can worsen daytime PTSD symptoms. Worse daytime symptoms can make nightmares more likely. Rinse and repeat [Germain, 2013].
And then your brain adds little “bonus features,” like:
- Rumination: trying to solve the nightmare like it’s a puzzle (spoiler: it’s usually not a puzzle, it’s a stress response).
- Catastrophizing: “This will never stop,” which ramps up nighttime anxiety.
- Sleep avoidance: because your bed starts feeling like enemy territory.
I don’t say that to scold you. Sleep avoidance makes complete emotional sense. It’s just a trap.
A serious note: chronic nightmares and safety
I’m going to be plain here, because you deserve clarity.
Chronic nightmares are associated with increased suicidal thoughts and behavior, including in people with PTSD, even when accounting for other factors like depression in some studies [Nadorff et al., 2011. Pigeon et al., 2012]. This does not mean nightmares “cause” suicide, and it does not mean statistics predict you as an individual. It means persistent sleep disturbance can grind people downand hopelessness can become dangerous.
If suicidal thoughts are in the mix, treat it as urgent and treatable.
If you’re in immediate danger, call your local emergency number now.
Crisis resources (U.S.):
- Call/Text 988 (Suicide & Crisis Lifeline)
- Veterans Crisis Line: 988, then press 1
- Crisis Text Line: Text HOME to 741741
- SAMHSA Helpline: 1-800-662-4357
Outside the U.S.:
- You can look up your country’s crisis line via the IASP directory or Befrienders Worldwide [IASP. Befrienders Worldwide].
If you tell me your country, I’ll help you find the right numbers.
The two treatments that actually have the receipts
There are lots of suggestions floating around the internet (some helpful, some vibes-only). But two options have especially solid evidence for PTSD-related nightmares:
- Prazosin (medication)
- Image Rehearsal Therapy (IRT) (therapy) [AASM Position Paper, 2018. VA/DoD, 2023]
I think of it like this:
- Prazosin can turn down the volume.
- IRT helps you change the channel.
Quick comparison table
| Option | What it targets | Evidence strength | Best for | Watch out for |
|—|—|—|—|—|
| IRT (Image Rehearsal Therapy) | Nightmare script + distress | Strong/Recommended for nightmare disorder, including PTSD-related nightmares [AASM Position Paper, 2018] | People who want skills that last beyond a medication | Can temporarily increase distress; best with a therapist if dissociation/self-harm risk |
| Prazosin (bedtime, prescription) | Nighttime hyperarousal/norepinephrine | Mixed but commonly used, some trials positive, at least one large trial negative [Raskind et al., 2007. Raskind et al., 2018] | Prominent nightmares, especially when hyperarousal is strong | Low blood pressure, dizziness/falls, interactions with other BP meds; requires clinician oversight |
| CBT-I (for insomnia) | Insomnia that fuels the cycle | Strong for insomnia; often helpful alongside PTSD care [AASM CBT-I Guideline, 2021] | Trouble falling/staying asleep even without nightmares every night | Needs structured program; may feel counterintuitive at first |
| Sleep apnea evaluation/CPAP (if needed) | Fragmented sleep + oxygen drops | Strong when apnea is present [AASM Guideline. Mysliwiec et al., 2015] | Snoring, choking/gasping, witnessed apneas, severe daytime sleepiness | Mask adjustment period; requires diagnosis + setup |
1) Prazosin: the “please let me sleep” option (with important nuance)
Prazosin is an alpha‑1 adrenergic blocker originally used for blood pressure. It’s often prescribed off-label for PTSD-related nightmares in many regions, based on its effects on adrenergic (noradrenergic) signaling at night [VA/DoD, 2023. Raskind et al., 2007].
What the evidence actually says: early studies and some meta-analyses found meaningful nightmare improvement for many patients, but results are not uniform, and a large randomized trial in veterans did not find a significant benefit over placebo on primary outcomes [Raskind et al., 2007. Raskind et al., 2018]. In real-world practice, some people do very well. Others get little benefit or can’t tolerate the side effects.
What people may notice: when it works, some people report improvement within days to a couple of weeks, while others need slower titration or don’t respond [VA/DoD, 2023].
How it’s taken (typical clinical approach): often at bedtime, usually starting low and titrating gradually while monitoring blood pressure and symptoms (your prescriber sets the schedule) [VA/DoD, 2023].
Big side effect to know: dizziness when standing (orthostatic hypotension), especially with the first doses or dose increases. Falls risk matters herespecially if you get up at night to use the bathroom [VA/DoD, 2023].
Medication interactions / “double-check with your pharmacist” moments:
- If you take other blood pressure medicines, alpha blockers, or PDE-5 inhibitors (e.g., sildenafil/tadalafil), the low-BP risk can be higherthis is specifically worth flagging before starting [VA/DoD, 2023].
- If you drink alcohol at night, it can worsen dizziness and sleep fragmentation.
If prazosin doesn’t work (or you can’t tolerate it): that’s not the end of the road. Clinicians may discuss:
- optimizing IRT and/or CBT-I,
- making sure sleep apnea isn’t undermining everything,
- or considering other off-label options based on your history (these vary by clinician and have less consistent evidence than IRT) [AASM Position Paper, 2018. VA/DoD, 2023].
Who should be extra careful with prazosin
Bring this up explicitly with your prescriber if any apply:
- Low blood pressure, fainting, frequent dizziness, or fall risk
- Older adults (nighttime falls matter)
- Pregnancy/breastfeeding (risk-benefit needs individualized review)
- Multiple medications affecting blood pressure (including PDE-5 inhibitors)
- Severe depression or active suicidality (not because prazosin “causes” it, but because you need a tightly coordinated safety plan)
2) Image Rehearsal Therapy (IRT): rewriting the nightmare on purpose (with safeguards)
IRT is exactly what it sounds like, and yes, it can feel a little weird at first. You’re basically telling your brain: “Cool story. We’re doing a rewrite.”
AASM and other expert groups list IRT as a first-line behavioral treatment for nightmare disorder, including PTSD-related nightmares [AASM Position Paper, 2018]. Meta-analyses and clinical trials generally show reductions in nightmare frequency and distress for many people, though results vary [Casement & Swanson, 2012. Krakow et al., 2001].
The basic idea:
- Write down the nightmare (you don’t need perfect details, just the core sequence).
- Create a new version where you have safety, control, or resolution.
- Rehearse the new version in your mind for 10-20 minutes a day for several weeks, ideally consistently [AASM Position Paper, 2018].
You’re not trying to pretend the trauma didn’t happen. You’re training your nervous system out of that automatic replay groove.
Timing: some people notice improvement within a few weeks. For others it’s more like 6-12 weeks for bigger, steadier change [AASM Position Paper, 2018. Casement & Swanson, 2012]. Many people find benefits persist after treatment ends.
IRT cautions (so you don’t accidentally make it harsher)
A few guardrails that matter:
- Don’t start with your most extreme nightmare if it’s likely to flood you. Start with a “medium-bad” one and build skill first.
- If you experience dissociation, self-harm urges, severe panic, or you feel unsafe when rehearsing, do IRT with a trauma-informed therapist and pause the solo work until you have support.
- If rehearsal temporarily increases distress, that can happenespecially earlybut it’s a sign to adjust the plan, not force your way through it [AASM Position Paper, 2018].
Can you do both (prazosin + IRT)?
Sometimes, yesand for a lot of people it’s a strong combo.
- Prazosin can give faster breathing room (when it works).
- IRT can build longer-term change in the nightmare script.
Needing both isn’t failure. It’s two tools for a complicated nervous system.
Also: “knock you out” sedatives aren’t always a good long-term strategy for PTSD nightmares, and some can complicate sleep architecture or trauma treatment. If meds are on the table, this is a good reason to work with a clinician who understands trauma + sleep [VA/DoD, 2023].
The plot twist: sometimes it’s sleep apnea
You came here for trauma nightmares and I’m about to talk about when nightmares signal trouble. But it matters.
Obstructive sleep apnea (OSA) appears to be common among people with PTSD and can worsen nightmares by fragmenting sleeespecially REMso your brain is basically trying to dream while repeatedly getting yanked toward wakefulness [Mysliwiec et al., 2015]. That’s a recipe for intense, sticky nightmares.
Get screened if you notice:
- loud snoring or someone sees you stop breathing
- waking up gasping/choking
- significant daytime sleepiness
- nightmares with drowning/breathing themes
- you’re doing “everything right” and nightmares aren’t budging
If apnea is part of the problem, CPAP (or other treatments) can reduce nightmares for some people simply by stabilizing sleep [Mysliwiec et al., 2015].
What to do tonight when you wake up in panic (the 3 a.m. plan)
If you’re reading this in the dark, with that post-nightmare adrenaline still buzzingfirst, I’m sorry. Second, you don’t need to “process” anything right now. You need to get your system out of emergency mode.
Here’s a simple sequence:
1) Keep it low and slow
Keep lighting dim. Stay in “downshift mode.”
Try 5-4-3-2-1 grounding:
- 5 things you see
- 4 things you can touch
- 3 things you hear
- 2 things you smell
- 1 thing you taste
It’s not magic. It’s a way to tell your brain, “We are here. In this room. In this year.”
2) Breathe like you mean it (but not in a perfectionist way)
A few slow belly breaths. While you do it, try one sentence of truth:
“That was a memory replaying. It’s not danger happening right now.”
Say it like you’re talking to a skittish dog. Calm, firm, repetitive.
3) Make one tiny safety tweak
Not a whole makeover. One tweak.
- a dim night light if darkness spikes anxiety
- white noise if every creak sends you into orbit
- a comforting object (yes, adults can have those)
4) If you’re still wired after ~20-30 minutes, get out of bed briefly
This breaks the association of bed = panic arena.
Do something boring and low-stimulation (avoid screens if you candoom-scrolling at 3 a.m. tends to crank up arousal). Go back to bed when you feel sleepy again.
Tonight doesn’t have to be perfect. It just has to be safer than the last 20 minutes.
The “boring but helpful” habits (pick two, not twelve)
Sleep hygiene isn’t a cure for PTSD nightmares, but it’s the foundation that helps everything else work better.
- Consistency: keep wake/sleep times within about 30-60 minutes most days.
- Caffeine earlier than you want: if you’re sensitive, afternoon coffee can absolutely haunt your night.
- Alcohol isn’t a sleep aid: it can knock you out and then reduce sleep quality later.
- Wind-down routine: even 10 minutes of something repetitive and calming helps your body get the memo.
- Progressive muscle relaxation: tense/release muscle groups before bed if your body is stuck in “ready to sprint.”
If you try a couple of these consistently for a few weeks and your sleep is still getting body-slammed, that’s not a character flawthat’s a sign you may need targeted treatment (IRT, prazosin discussion, CBT-I, and/or apnea screening) [AASM CBT-I Guideline, 2021. AASM Position Paper, 2018].
When it’s time to bring in a professional (aka: when you stop white-knuckling it)
You deserve backup if:
- nightmares happen multiple times a week and impair your day
- you’re avoiding sleep on purpose
- you’re using alcohol/substances to block dreams
- you have any suicidal thoughts (even “passing” ones)
- you’re having major functioning problems from sleep loss
- you’ve tried self-help changes for 4-6 weeks and nothing is improving
And please get medical evaluation promptly if:
- insomnia or nightmares are persisting >>3 weeks with significant distress or impairment
- you suspect sleep apnea (snoring, choking, breathing pauses)
- you regularly wake gasping/choking
- you have violent sleep behaviors, injuries, or may be acting out dreams
- you’re so sleepy during the day that it affects driving, work safety, or parenting safety [AASM ICSD-3]
What recovery actually looks like (so you don’t quit in the messy middle)
A lot of people see real improvement with treatmentsometimes dramatic improvement. Nightmare frequency and distress often decrease with targeted nightmare therapy and/or effective PTSD treatment, though some people have lingering symptoms and need a combined approach [AASM Position Paper, 2018. VA/DoD, 2023].
Also: if you start trauma-focused therapy, sleep can temporarily get worse before it gets better. That doesn’t mean you’re broken or therapy “failed.” It can be part of the process as your brain finally opens the file it’s been keeping locked in a drawer [VA/DoD, 2023].
The win isn’t always “never have a nightmare again.” Sometimes it’s:
- fewer nightmares,
- less intensity,
- you fall back asleep faster,
- your next day isn’t wrecked.
That’s not “settling.” That’s your nervous system learning it doesn’t have to run security drills every night.
You don’t have to get used to surviving the night
PTSD nightmares are common, brutal, and treatable. If your brain has been running the same terrifying clip on repeat, it’s not because you’re weakit’s because your system is stuck in protection mode.
Start with what you can do tonight. Then, if this has been going on for a while, consider talking to a clinician about:
- Image Rehearsal Therapy (IRT) (a top evidence-based option),
- prazosin (a common off-label option with mixed-but-real-world usefulness for some),
- CBT-I if insomnia is feeding the cycle,
- and sleep apnea screening (because oxygen matters more than we like to admit).
You deserve sleep that doesn’t feel like a battlefield. And you don’t have to figure it out alone.
Frequently Asked Questions
Do PTSD nightmares mean I’m getting worse?
Not necessarily. Nightmares can flare with stress, triggers, changes in sleep schedule, or when you begin trauma-focused therapy. What matters most is the overall trend over time and whether you’re becoming safer, more supported, and more functionalnot whether you had a bad night.
Does prazosin actually work for PTSD nightmares?
For some people, yesbut the research is mixed. Earlier studies showed improvements, while a large randomized trial in veterans did not find a significant benefit on primary outcomes [Raskind et al., 2018]. It’s still commonly discussed as an option because individual response can be meaningful, and clinicians can monitor safety and adjust the plan.
What dose of prazosin is used for nightmares?
Dosing is individualized and should be managed by a prescriber. Many clinicians start low at bedtime and titrate gradually while monitoring blood pressure, dizziness, and response [VA/DoD, 2023]. If you’re prone to fainting, falls, or low blood pressure, make sure that’s part of the conversation.
How long does Image Rehearsal Therapy (IRT) take to work?
Some people notice improvement within a few weeks, but many need consistent practice for several weeks to a few months to see bigger changes [AASM Position Paper, 2018]. Doing it with a therapist can make it easier to stick with and adjust if distress spikes.
When should I practice IRT right before bed or during the day?
Most people do best practicing during the day (or early evening) rather than right at bedtimeespecially if rehearsal stirs up emotion. The goal is steady repetition, not ramping up arousal right before sleep.
What if I have diabetes, GERD, or I’m on other medicationsdoes any of this change?
The big issue here is usually medication interactions and blood pressure, not food rules. If you take blood pressure meds, alpha blockers, or PDE‑5 inhibitors, prazosin needs extra caution and pharmacist/clinician review [VA/DoD, 2023]. If reflux or blood sugar swings wake you at night, addressing those conditions can still meaningfully reduce sleep fragmentation (which can lower nightmare frequency indirectly).
When should I see a doctor (or sleep specialist) about nightmares?
Seek professional help if nightmares happen multiple times a week for >>3 weeks, if you’re avoiding sleep, using substances to suppress dreams, waking gasping/choking, injuring yourself or a bed partner, or if daytime sleepiness affects safety. If you have suicidal thoughts, seek urgent support the same day (988 in the U.S., or your local emergency/crisis line) [Nadorff et al., 2011. AASM ICSD-3].
Sources
- Germain, A. “Sleep Disturbances as the Hallmark of PTSD: Where Are We Now?” American Journal of Psychiatry, 2013. (review)
- American Academy of Sleep Medicine. International Classification of Sleep Disorders (ICSD-3), 2014. (diagnostic manual/overview)
- Raskind, M.A., et al. “A Trial of Prazosin for Combat Trauma PTSD With Nightmares.” Biological Psychiatry, 2007. (randomized trial)
- Raskind, M.A., et al. “Trial of Prazosin for Post-Traumatic Stress Disorder in Military Veterans.” New England Journal of Medicine, 2018. (randomized trial)
- U.S. Department of Veterans Affairs / Department of Defense. VA/DoD Clinical Practice Guideline for the Management of Posttraumatic Stress Disorder and Acute Stress Disorder, 2023. (guideline) https://www.healthquality.va.gov/
- Aurora, R.N., et al. “Best Practice Guide for the Treatment of Nightmare Disorder in Adults.” Journal of Clinical Sleep Medicine, 2010. (guideline)
- American Academy of Sleep Medicine. “Position Paper / Guidance on Nightmare Disorder Treatments (including IRT).” Journal of Clinical Sleep Medicine, 2018. (position paper)
- Casement, M.D., & Swanson, L.M. “A Meta-Analysis of Imagery Rehearsal for Post-Trauma Nightmares.” Journal of Anxiety Disorders, 2012. (meta-analysis)
- Krakow, B., et al. “Imagery Rehearsal Therapy for Chronic Nightmares in Sexual Assault Survivors with PTSD.” JAMA, 2001. (clinical trial)
- Mysliwiec, V., et al. “Sleep Disorders in US Military Personnel: A High Rate of Comorbid Insomnia and Obstructive Sleep Apnea.” Chest, 2015. (observational study)
- Edinger, J.D., et al. “Behavioral and Psychological Treatments for Chronic Insomnia Disorder in Adults: An American Academy of Sleep Medicine Clinical Practice Guideline.” Journal of Clinical Sleep Medicine, 2021. (guideline)
- Nadorff, M.R., et al. “Nightmares and Suicidality: A Meta-Analysis.” Sleep, 2011. (meta-analysis)
- Pigeon, W.R., et al. “Sleep Disturbance Preceding Suicidal Ideation/Behavior (nightmares/insomnia associations).” Journal of Clinical Sleep Medicine, 2012. (observational study)
- International Association for Suicide Prevention (IASP). “Crisis Centres / Helplines by Country.” https://www.iasp.info/resources/Crisis_Centres/ (resource directory)
- Befrienders Worldwide. “Find a Helpline.” https://www.befrienders.org/ (resource directory)