Written by [Author Name]. Medically reviewed by [Reviewer Name, MD] (Emergency Medicine/Cardiology). Last updated: 2025-12-23.
Chest pain is the absolute worst kind of “fun surprise.” It’s like your body decided to throw you a pop quiz with no study guide, and the answer options are: “anxiety” or “call an ambulance.”
The short answer: If chest pain is new, severe, feels like pressure/squeezing, comes with shortness of breath/sweating/nausea, or spreads to your arm/jaw/back call 911. Don’t try to “logic” your way through it.
Key exception: If this perfectly matches your known panic pattern and you have no red flags, it may be a panic episode but you still should get checked if anything is new/different.
When it matters less: If you’ve been evaluated before and told it’s panic or another non-cardiac cause, you can focus more on management but any change in pattern deserves re-checking.
I’m not your doctor, and this isn’t medical advice this is me, a fellow human, trying to help you sort the “this is scary but probably not deadly” from the “this is scary and we need help right now.”
First: When to Call 911 (No Debates, No Polling the Group Chat)
If you take one thing from this post, make it this: if you’re not sure, it’s okay to get checked. Chest pain is one of those symptoms you don’t “power through” to prove a point because the downside of being wrong is high [AHA Heart Attack Symptoms. 2021 AHA/ACC Chest Pain Guideline].
Call 911 immediately if any of these are true:
- This is the first time you’ve ever felt this kind of chest pain/pressure
- The sensation spreads to your arm, jaw, neck, shoulder, or back
- You’re fainting, feel like you might pass out, or you’re drenched in cold/clammy sweat
- You have severe shortness of breath that isn’t easing
- It lasts more than a few minutes, doesn’t improve with rest, or goes away and comes back [AHA Heart Attack Symptoms. CDC Heart Attack Signs]
- It feels like squeezing/heavy pressure (not just a quick jab) and it’s sticking around
- It started during or right after physical activity (stairs, shoveling, exercise, etc.)
Also call 911 now for chest pain plus any of these “don’t miss” danger signs (they can signal other emergencies besides a heart attack):
- Sudden severe “tearing” chest/back pain, or chest pain with new weakness/numbness, trouble speaking, or facial droop (think: aortic catastrophe or stroke symptoms)
- One sided leg swelling, coughing up blood, or sudden unexplained shortness of breath (possible blood clot in the lung)
- Sudden sharp chest pain + major trouble breathing (possible collapsed lung)
- A very fast/irregular heartbeat with lightheadedness or fainting [2021 AHA/ACC Chest Pain Guideline]
Call even sooner if you have higher risk context, like: known heart disease (prior heart attack, stent, bypass), diabetes, kidney disease, smoking, high blood pressure, high cholesterol, strong family history of early heart disease, or you’re older (risk rises with age) [CDC Heart Attack Signs. 2021 AHA/ACC Chest Pain Guideline].
While you’re waiting for the ambulance (quick, practical)
- Don’t drive yourself. EMS can start care on the way and is safer if you collapse or your rhythm changes [AHA Heart Attack Symptoms].
- Sit down, rest, and unlock your door (or have someone meet EMS).
- If you’ve been prescribed nitroglycerin, take it only as directed for chest pain and tell EMS what you took.
- Aspirin: Some emergency guidance recommends chewing aspirin for suspected heart attack if you’re not allergic and have no known major bleeding risk but if you can, follow your local emergency dispatcher’s instructions first (they’ll factor in your situation) [AHA Heart Attack Symptoms].
- If you’re alone, call someone to stay on the line until help arrives.
If none of those red flags fit and this feels like something you’ve experienced before, keep reading but please hear me: when in doubt, get checked out.
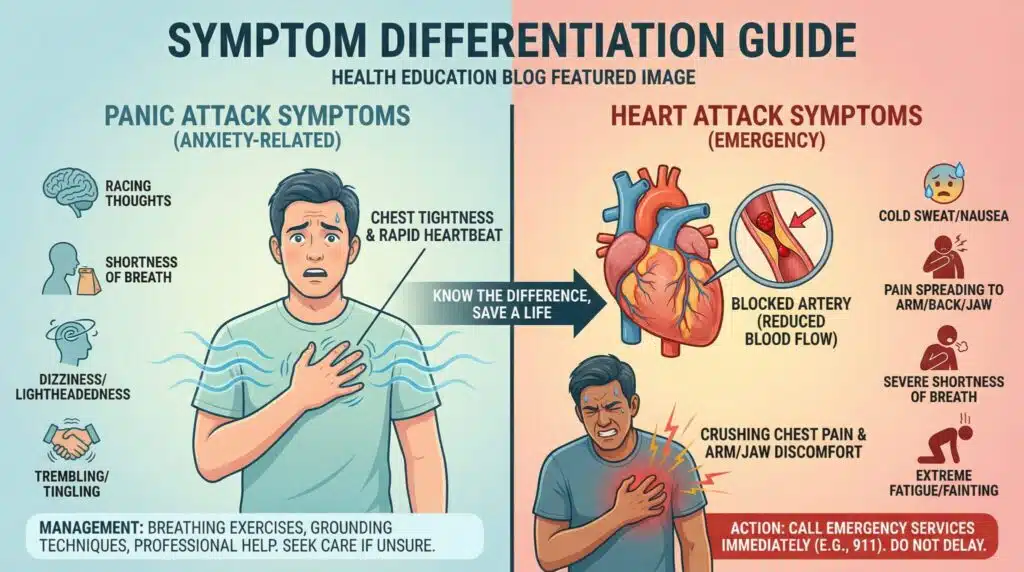
Why Panic Attacks and Heart Attacks Feel Weirdly Similar
Both can mess with your breathing. Both can make your heart race. Both can make you sweat and feel like the world just tilted 10 degrees to the left.
The difference is the “why”:
- Panic attack: your nervous system hits the gas pedal (fight or flight/adrenaline surge), which can cause chest tightness, racing heart, tingling, and a sense of doom [APA DSM-5-TR].
- Heart attack: blood flow in a coronary artery is blocked or reduced enough that part of the heart muscle isn’t getting enough oxygen [CDC Heart Attack Signs].
And here’s the rude plot twist: heart problems aren’t always dramatic. Sometimes it’s “just” pressure or heaviness people brush off as stress or heartburn. Meanwhile panic can feel sharp and terrifying and very “movie heart attack.”
So yeah confusing. Let’s talk patterns.
What a Panic Attack Often Feels Like (The “My Body Is Yelling” Experience)
Panic attacks can be intensely physical like your body found the emergency alarm button and then snapped it off.
Common panic patterns:
- Sharp, stabbing, or “surface level” chest pain (often, not always)
- Discomfort that often stays centered (not radiating though panic can feel weird and widespread)
- Fast, shallow breathing, shaking, tingling in hands/lips, sweating, hot/cold flushes
- A racing heart you can feel pounding
- Often starts at rest, during stress, or can even wake you from sleep
- Symptoms that peak within minutes and then gradually ease (many people feel the worst within ~10 minutes, though after effects can linger) [APA DSM-5-TR]
One reason people spiral is because panic makes you scan for danger… which makes you notice every sensation… which makes you more panicked… which makes the sensations louder. It’s like a microphone feeding back except the microphone is your chest.
A quick breathing “reset” you can try (only if you have no red flags)
This isn’t a diagnosis. It’s just a way to nudge your nervous system toward “we’re safe.”
Try paced breathing (gentler than big breath holds):
- Inhale through your nose for 4
- Exhale slowly for 6
- Repeat for 2-3 minutes
Stop if you feel more dizzy, more tingly, or more “air hungry.” If you tend to hyperventilate, smaller/softer breaths can work better than deep ones.
If you have COPD/asthma or wheeze: try pursed lip breathing (inhale gently through the nose, exhale longer through pursed lips). If breathing is severely difficult, that’s an emergency get help.
Important: even if breathing helps, that doesn’t prove it’s not your heart. Consider it a tool, not a verdict.
What a Heart Attack Often Feels Like (The “Deep Pressure” Situation)
Heart attack symptoms are often described less like a jab and more like deep heaviness tightness, pressure, squeezing, “an elephant on my chest” [AHA Heart Attack Symptoms. CDC Heart Attack Signs].
Common heart attack patterns:
- Deep pressure or tightness in the chest (more than a quick sharp stab)
- Discomfort that can spread to the arm (often left), jaw, neck, shoulder, or back
- Cold, clammy sweating, nausea/vomiting, or a sudden “something is really wrong” feeling
- Often triggered by exertion (stairs, exercise, physical work) but can happen at rest [2021 AHA/ACC Chest Pain Guideline]
- Symptoms that persist, build, or come in waves without fully resolving
A note for women (and anyone with atypical symptoms): not everyone gets the classic chest pressure story. Some people especially women may have warning signs like unusual fatigue, lightheadedness, nausea, jaw/shoulder pain, or shortness of breath with minimal or no chest pain [AHA Heart Attack Symptoms]. If that’s new or persistent, please don’t let anyone (including your own brain) talk you out of getting checked.
The Quick “Pattern Check” (Because Fear Makes Your Brain Forget Everything)
In the moment, you don’t need a medical dissertation. You need a simple gut check:
- More like panic (often): sharp + centered + peaks fast + often at rest/stress
- More like heart (often): deep pressure + spreads + triggered by exertion + doesn’t go away
If you’ve got spreading pain, an exertion trigger, or persistent symptoms, that’s your cue to get emergency help. Patterns beat guesses.
A simple decision rule: If you’re thinking “Should I call?” and you can’t confidently say “This is my usual panic pattern and I have zero red flags,” call 911 [AHA Heart Attack Symptoms].
If It’s a Panic Episode: How to Ride It Out Without Making It Worse
If you’re sure you have no red flags and this matches your known panic pattern, the goal is simple: stay safe, help your body downshift, and keep an eye out for anything that changes.
Things that tend to help:
- Keep breathing slow (paced breathing, not big gulping breaths)
- Grounding: name 5 things you see, 4 you can touch, 3 you hear (give your brain a job)
- Reality talk: “This feels awful, but it’s a panic wave. It rises, peaks, and falls.”
Switch to “urgent evaluation in the ER” mode if:
- chest pain changes character (new pressure, new spreading)
- you faint / nearly faint
- you have new severe shortness of breath
- you blow past your usual panic timeframe with no improvement
- anything feels meaningfully new, different, or “off”
Your job isn’t to “win” against symptoms. Your job is to be safe.
If You Go to the ER: What They’ll Usually Do (So It’s Less Scary)
The ER is built for this exact mystery: “Is it my heart or something else?”
Typically, they’ll do:
- EKG/ECG early on to look for rhythm problems or signs of reduced blood flow [2021 AHA/ACC Chest Pain Guideline]
- Blood tests, including high sensitivity troponin, which can rise when heart muscle is injured [2021 AHA/ACC Chest Pain Guideline]
- Repeat testing over a few hours if needed, because not everything shows up instantly [2021 AHA/ACC Chest Pain Guideline]
And yes if it’s “just” panic, you didn’t waste anyone’s time. The testing exists to rule out dangerous stuff.
After You Know What It Was: Your Next Step
Once you have an answer, the spiral loses a lot of power. (Answers are calming even if the waiting room chairs are not.)
If it was panic: it’s treatable, and you deserve support. Therapy (especially CBT) helps many people, and some folks also benefit from medication your clinician can help you match the plan to your symptoms and medical history [NICE CG113].
If it was a heart issue: follow up care matters meds, cardiac rehab, risk factor management, the whole “take your heart seriously” era. Fast treatment is one reason calling EMS quickly matters [AHA Heart Attack Symptoms].
One practical tip either way: write down what happened while it’s fresh what you were doing, how it felt (sharp vs pressure), whether it spread, how long it lasted, what helped, and what made it worse. Bringing that to your clinician is weirdly helpful when your memory is fuzzy from adrenaline.
Who Should Be Extra Careful About “It’s Probably Just Anxiety”
A few groups deserve a lower threshold to seek urgent evaluation for chest pain/shortness of breath:
- Diabetes: heart problems can present with less “classic” chest pain (don’t wait for the movie version) [CDC Heart Attack Signs].
- Pregnancy and postpartum (especially the first weeks after delivery): clot risk is higher, and shortness of breath/chest pain should be taken seriously.
- Known heart disease (prior heart attack, stent, bypass) or prescribed nitroglycerin: treat new or changing symptoms as urgent [2021 AHA/ACC Chest Pain Guideline].
- Recent stimulant/cocaine/amphetamine use: chest pain needs emergency evaluation because it can trigger dangerous heart and vessel problems [AHA Scientific Statement, 2008].
- Recent viral illness (or chest pain worse with deep breaths/lying flat): myocarditis/pericarditis can mimic other causes and should be assessed, especially if symptoms are new or worsening [NHS Myocarditis/Pericarditis Overview].
Panic vs Heart Attack (Quick Comparison Table)
| Feature | Panic attack (often) | Heart attack (often) | What to do |
|---|---|---|---|
| Pain quality | Sharp, stabbing, tightness. Can feel “surfacey” | Pressure, squeezing, heaviness | If pressure/squeezing or severe pain: call 911 [AHA Heart Attack Symptoms] |
| Onset | Often sudden, may follow stress. Can happen at rest | Can be during exertion or at rest | Exertional onset is a red flag [2021 AHA/ACC Chest Pain Guideline] |
| Duration | Peaks within minutes. May ease over 20-60 min (after effects can linger) | Persists, builds, or comes and goes without fully resolving | If it lasts more than a few minutes or returns: call 911 [CDC Heart Attack Signs] |
| Spreading pain | Less common | More common (arm/jaw/neck/back) | Spreading pain = emergency |
| Other symptoms | Tingling, trembling, fear, feeling unreal | Sweating, nausea, shortness of breath, “impending doom” | Either can feel terrifying use red flags, not vibes |
Frequently Asked Questions
How can I tell if chest pain is anxiety or a heart attack?
You usually can’t tell with certainty at home because symptoms overlap. Use red flags: new pain, pressure/squeezing, spreading pain, fainting, severe shortness of breath, or symptoms that last more than a few minutes or keep returning = call 911 [AHA Heart Attack Symptoms. CDC Heart Attack Signs].
How long should I wait before calling 911 for chest pain?
If symptoms are severe, new, or include red flags, don’t wait. Many public health recommendations use “more than a few minutes” or “goes away and comes back” as the threshold for emergency help [AHA Heart Attack Symptoms].
Can a panic attack cause chest pain for hours?
The most intense part often peaks within minutes, but muscle soreness, lingering adrenaline, and ongoing anxious breathing can make discomfort feel like it drags on. The key is pattern: if it’s different from your usual, worsening, or paired with red flags, get evaluated.
Should I chew aspirin if I think I’m having a heart attack and how much?
Some guidance suggests chewing aspirin while waiting for EMS if you’re not allergic and don’t have a known major bleeding risk, but it’s best to follow 911/dispatcher instructions because they can tailor advice to you [AHA Heart Attack Symptoms]. If you’ve been told not to take aspirin, don’t.
Is it safe to do breathing exercises during chest tightness?
Gentle paced breathing (like 4-in/6-out) is generally safer than long breath holds if you’re prone to hyperventilation. Stop if it worsens dizziness, tingling, or “air hunger,” and seek urgent care for severe or worsening shortness of breath.
What if I have GERD, diabetes, I’m pregnant/postpartum, or I take heart medications?
GERD can mimic chest pain, but new/severe symptoms still need evaluation especially if you have shortness of breath, sweating, or exertional triggers. Diabetes and pregnancy/postpartum are reasons to have a lower threshold to seek urgent care. If you take nitroglycerin or have known heart disease, treat changing symptoms as urgent [2021 AHA/ACC Chest Pain Guideline].
When should I talk to a clinician about this (even if it wasn’t a heart attack)?
Get follow up if you have recurrent chest pain, panic episodes that limit your life, or you’re avoiding activity out of fear. Seek urgent evaluation sooner if you have fainting, palpitations with near fainting, chest pain with neurologic symptoms (weakness, trouble speaking), or suspected sleep apnea symptoms and nighttime panic worries like waking up gasping/choking.
If you’re sitting there right now with symptoms and uncertainty: please choose the safe option and get help. You can be anxious and smart. Those two things can absolutely coexist.
Sources
- Gulati M, Levy PD, Mukherjee D, et al. “2021 AHA/ACC/ASE/CHEST/SAEM/SCCT/SCMR Guideline for the Evaluation and Diagnosis of Chest Pain.” Circulation, 2021. (guideline)
- American Heart Association (AHA). “Heart Attack Symptoms.” https://www.heart.org/ (overview)
- Centers for Disease Control and Prevention (CDC). “Heart Attack Symptoms.” https://www.cdc.gov/ (overview)
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM-5-TR). American Psychiatric Publishing, 2022. (reference)
- National Institute for Health and Care Excellence (NICE). “Generalised anxiety disorder and panic disorder in adults: management (CG113).” https://www.nice.org.uk/guidance/cg113 (guideline)
- American Heart Association (AHA). “Management of Cocaine Associated Chest Pain and Myocardial Infarction.” Circulation, 2008. (scientific statement)
- National Health Service (NHS). “Myocarditis” / “Pericarditis.” https://www.nhs.uk/ (overview)