Waking up at 2:17 a.m. with your heart doing parkour in your ribcage is… not the cozy bedtime vibe anyone ordered. You’re sweaty, your brain is yelling “DANGER,” and you’re sitting there like, “Cool cool cool was that a night terror or a panic attack?”
The short answer: If you remember it clearly, it often points to a nocturnal panic attack. If you have little to no memory and someone else witnessed you acting terrified, it often points to a night terror (an NREM parasomnia) [AASM ICSD-3-TR, 2023. APA DSM-5-TR, 2022].
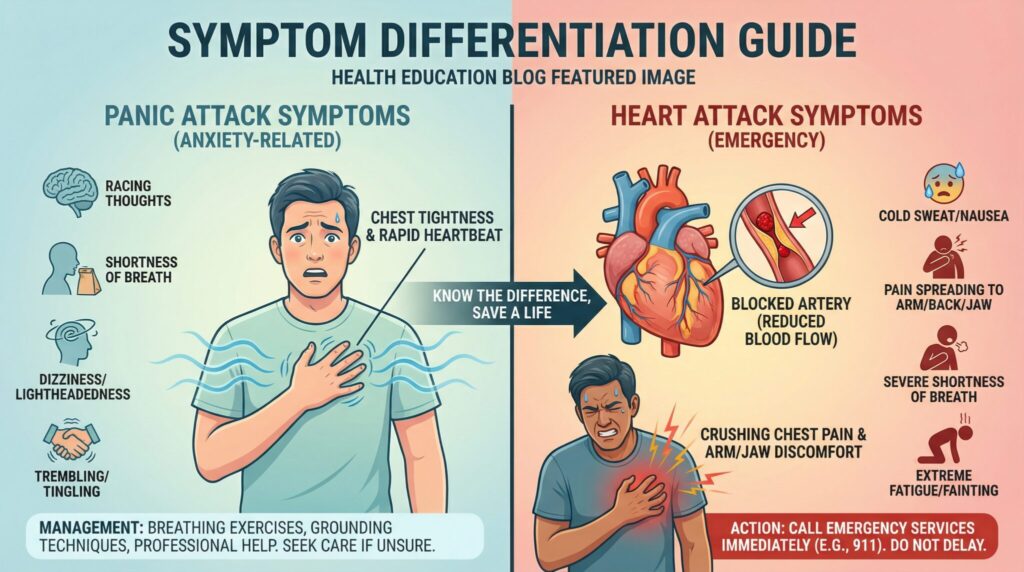
Key exception: If your main issue is gasping/choking, chest pain, or fainting, don’t self label get evaluated to rule out things like sleep apnea, reflux related laryngospasm, arrhythmia, or seizures [AASM Sleep Apnea Overview. AHA Heart Attack Warning Signs].
When it matters less: If it’s rare, brief, and you recover fully, you can often start with a simple log and bring it to your clinician no 47 tab spiral required.
It’s one question:
Do you remember it?
Like, do you have a clear “receipt” for what just happened… or is your brain handing you a blank piece of paper and shrugging?
First: the boring but important safety disclaimer (sorry)
This can be educational, but it can’t diagnose you. If anything about your episode feels medically sketchy, don’t “wait and see” to be brave.
Get emergency care now if you have:
- Chest pain/pressure, especially if it spreads to the arm, jaw, back, or comes with sweating, nausea, or a “something is very wrong” feeling [American Heart Association Heart Attack Warning Signs]
- Fainting, new severe weakness, or severe shortness of breath
- Loss of consciousness
- New neurologic signs (confusion that doesn’t clear, one sided weakness), or seizure like signs (stiffening, rhythmic jerking, tongue biting, incontinence) [NINDS Seizures Overview]
- Symptoms that are persistent/worsening, unusually intense for you, or not improving the way your typical episodes do
Okay. Now that we’ve put the “please don’t ignore a real emergency” sign in neon lights…
The memory trick: your brain’s “receipt” tells you the store
Here’s the quick and dirty difference:
- If you remember the episode you woke up, you knew you were terrified, you can describe it later this leans toward a nocturnal panic attack [APA DSM-5-TR, 2022].
- If you have little to no memory and someone else tells you you were crying/screaming/thrashing/bolting upright this leans toward a night terror [AASM ICSD-3-TR, 2023].
Why? Because night terrors are NREM parasomnias your brain is partly stuck between deep sleep and waking. Your body can go full alarm mode, while your “thinking brain” isn’t fully online [AASM ICSD-3-TR, 2023].
Panic attacks are different. You’re awake enough to experience the fight or flight surge (racing heart, doom feeling, shaking), and you can typically recall it afterward [APA DSM-5-TR, 2022].
The 2 Minute Memory Test (mini protocol)
Answer each one A or B. No overthinking.
1) Afterward, do you have a clear memory “receipt”?
- A: Not really / patchy / blank
- B: Yes, vivid and specific
2) During it, were you responsive to other people?
- A: Hard to wake, confused, pushed people away, didn’t “track”
- B: Awake enough to talk, explain, text, or orient to the room
3) What was the vibe of your body on the outside?
- A: Sitting up/bolting/thrashing/trying to run
- B: Mostly still, but internally feeling like a catastrophe
4) What happened afterward?
- A: Settled back down fairly fast. Minimal memory in the morning
- B: Wide awake, shaken, scanning for danger, afraid to fall back asleep
Mostly A → night terror pattern is more likely [AASM ICSD-3-TR, 2023]
Mostly B → nocturnal panic pattern is more likely [APA DSM-5-TR, 2022]
Mixed/unclear → consider confounders (next section) and talk with a clinician sometimes it takes a sleep history and occasionally a sleep study to untangle.
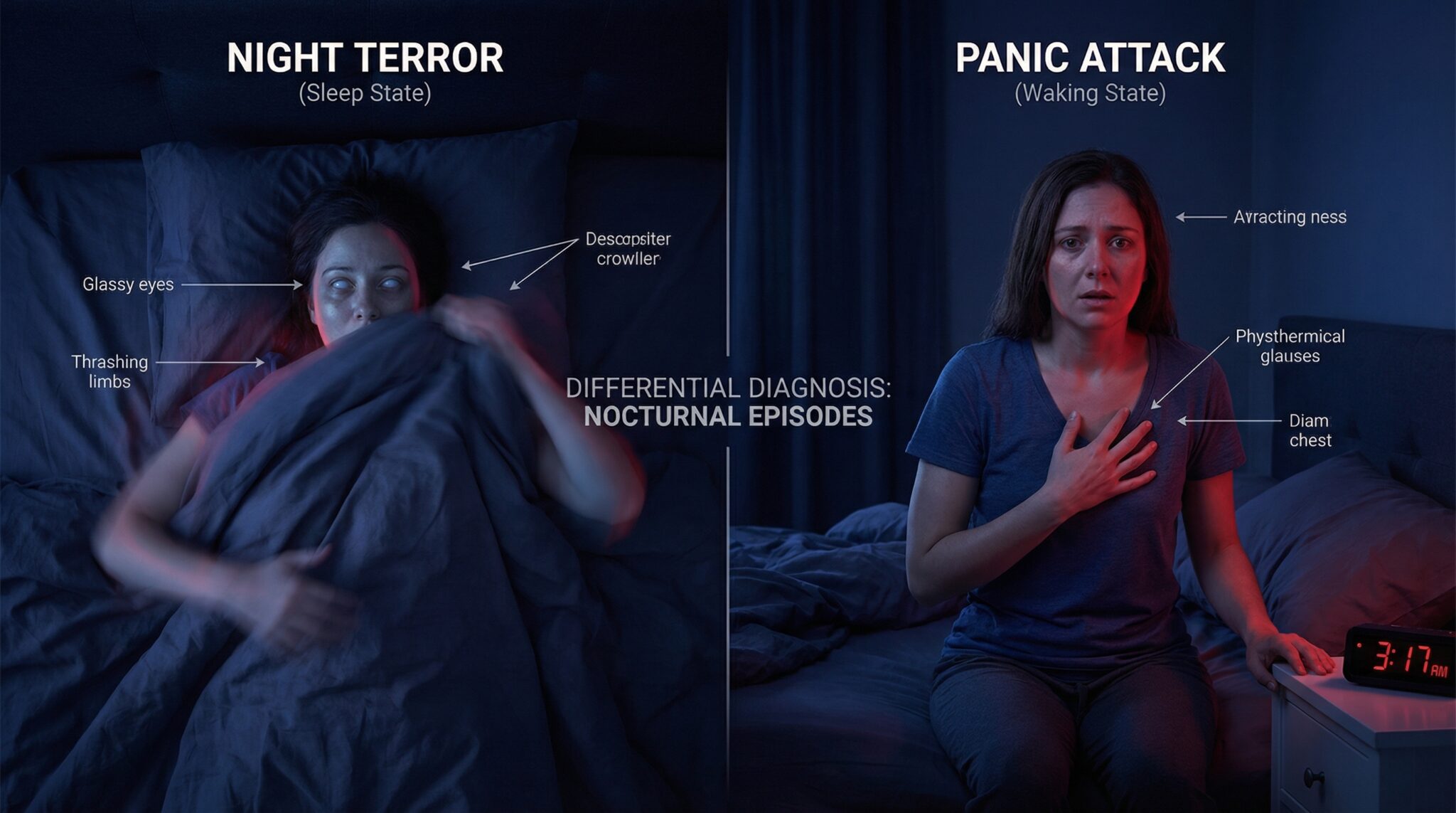
Night terrors vs nocturnal panic attacks (one screen comparison)
| Clue | Night terrors (NREM parasomnia) | Nocturnal panic attacks |
|---|---|---|
| Memory afterward | Often little/none [AASM ICSD-3-TR, 2023] | Often clear recall [APA DSM-5-TR, 2022] |
| Responsiveness | Hard to wake. Confused if woken | Awake/aware enough to describe it |
| What others see | Can be loud: screaming, thrashing, bolting | Often quieter externally. Intense internal fear |
| Timing | Often first third of the night (deep NREM) [AASM ICSD-3-TR, 2023] | Can occur from sleep, often in later/transition periods (varies) |
| Aftermath | Often settles quickly. May go back to sleep | Often stays awake. “Fear of sleep” can build |
| What helps in the moment | Safety + minimal stimulation | Grounding + slower breathing + reassurance |
| Who to see | Often sleep medicine | Often mental health clinician (and/or primary care) |
What it looks like on the outside (aka: what your poor household witnesses)
If you live alone, this section may feel like reading a review of a movie you didn’t know you starred in. If you have a partner? Congratulations, you have a very tired “nighttime narrator.”
Night terrors tend to be loud
People may:
- scream, thrash, sit up suddenly, bolt out of bed, even run
- have eyes open but look glassy/unfocused
- not respond normally to their name
- make sounds that aren’t really coherent speech
(These are classic NREM parasomnia features, especially in kids, but adults can have them too.) [AASM ICSD-3-TR, 2023]
Nocturnal panic attacks are often quieter externally but brutal internally
You might:
- stay mostly in bed, but feel like something is seriously wrong
- have racing heart, sweating, trembling
- feel chest pressure, nausea, dizziness
- be able to talk clearly (“I can’t breathe,” “Something’s happening,” etc.) [APA DSM-5-TR, 2022]
Important breathing note: If gasping/choking is a big feature (especially with loud snoring, witnessed pauses in breathing, or major daytime sleepiness), don’t just file it under “panic.” Sleep apnea and other breathing related sleep disorders are common and treatable and worth ruling out [AASM Sleep Apnea Overview]. Reflux related laryngospasm can also cause sudden “can’t breathe” awakenings in some people [Cleveland Clinic Laryngospasm].
The clock clue: when it happens matters (but isn’t perfect)
Your glowing nightstand clock isn’t just there to shame you with the time. It can help with caveats including why nights feel worse.
- Night terrors often happen earlier in the night, frequently in the first third during deep NREM sleep [AASM ICSD-3-TR, 2023].
- Nocturnal panic attacks can happen after falling asleep or during awakenings and may be noticed later at night but timing alone isn’t diagnostic [APA DSM-5-TR, 2022].
Aftermath patterns:
- After a night terror, many people settle back down relatively quickly (sometimes without fully “coming to”) [AASM ICSD-3-TR, 2023].
- After a panic attack, you’re more likely to be wide awake, trying to calm down plus that unfair side quest called “fear of going to sleep because what if it happens again.”
Yes, brains are rude.
My “middle of the night detective” checklist (no trench coat required)
If you’re trying to label what happened, run through these:
1. Do you remember it clearly?
Remember = panic leaning. No memory = night terror leaning. [AASM ICSD-3-TR, 2023. APA DSM-5-TR, 2022]
2. Were you fully awake/aware during it?
Awake and alert = panic leaning. Foggy/offline = night terror leaning.
3. Were you having specific fear thoughts (survival during sleep panic, heart attack, losing control)?
That’s very panic coded [APA DSM-5-TR, 2022].
4. What did your body do?
Running/thrashing/screaming = night terror leaning. Mostly still in bed with internal “oh no” = panic leaning.
5. Was breathing/choking the main thing?
Could be panic but also a big “rule out” flag for sleep apnea or reflux/laryngospasm, especially if it’s recurrent [AASM Sleep Apnea Overview. Cleveland Clinic Laryngospasm].
6. How fast did you fall back asleep?
Quickly = night terror leaning. Long, anxious, wired = panic leaning.
If your clues are messy or mixed, you’re not failing the quiz. Some people experience more than one thing and sometimes it takes a clinician (and occasionally a sleep study) to untangle it.
What else could it be? (common confounders to rule out)
Because “night terror vs panic” isn’t the only fork in the road.
- Obstructive sleep apnea (OSA): Loud snoring, witnessed pauses/gasping, morning headaches, major daytime sleepiness. Awakenings can feel like panic [AASM Sleep Apnea Overview].
- GERD / reflux related laryngospasm: Sudden choking/can’t breathe feeling, sour taste, burning, worse after late meals/alcohol. Ask about reflux treatment and timing [Cleveland Clinic Laryngospasm].
- Nocturnal seizures: Recurrent stereotyped events, tongue biting/incontinence, confusion afterward, injuries, or odd repetitive movements. Needs medical evaluation [NINDS Seizures Overview].
- Nightmares / PTSD nightmares: Typically REM related, often with clearer dream recall than night terrors. Daytime trauma symptoms may be present [AASM ICSD-3-TR, 2023].
- REM sleep behavior disorder (RBD): Dream enactment (punching/kicking), often later night REM. More common in older adults and deserves medical attention [Mayo Clinic REM Sleep Behavior Disorder].
- Medication/substance effects: Alcohol (especially withdrawal), cannabis changes, stimulants, decongestants, steroids, some antidepressants can affect sleep/arousal. Review timing/doses with a clinician/pharmacist.
- Thyroid/cardiac rhythm issues: Palpitations, tremor, weight change, heat intolerance, or episodes also happening in daytime worth a medical check.
- Low blood sugar (especially with diabetes meds): Night sweats, shakiness, morning headaches. Discuss safe overnight glucose targets with your clinician.
Who should be extra careful (quick edge case notes)
- If you have reflux: avoid big/fatty/spicy meals and alcohol close to bed. Consider head of bed elevation. Mention choking awakenings to your clinician [Cleveland Clinic Laryngospasm].
- If you’re monitoring blood sugar / on insulin or sulfonylureas: recurrent night sweats/shakiness warrant a glucose check plan with your diabetes clinician (don’t guess).
- If you take stimulants, steroids, thyroid meds, or activating antidepressants: ask whether timing/dose could be worsening nighttime surges.
- If you’re pregnant/postpartum: new shortness of breath, chest pain, fainting, or sudden panic like episodes deserve prompt medical review (rule outs matter).
- If there’s any seizure history or new “seizure ish” features: prioritize medical evaluation [NINDS Seizures Overview].
What to do in the moment (because flailing is not a strategy)
Let’s talk about what actually helps when you’re in it.
If it’s a panic attack: you’re awake, so you can steer
Your nervous system is basically a smoke alarm going off because you made toast. The goal is to send “we’re safe” signals not argue with the alarm like it’s a rational roommate.
- Ground yourself (fast).
Try 5-4-3-2-1: 5 things you see, 4 you can touch, 3 you hear, 2 you smell, 1 you taste. - Breathe with a longer exhale.
Many people find this easier than breath holds at 2 a.m.: inhale 4, exhale 6 (or inhale 3, exhale 5). Repeat for a few minutes.
If breath holding makes you feel worse, skip it. - Name it.
“This feels like a panic attack. I’m safe. This will peak and pass.“
Cheesy, yes. Also a useful counterweight to the doom narrative [APA DSM-5-TR, 2022]. - If you’re too wired to sleep, get up briefly.
Keep lights dim. Do something boring calm for 10-20 minutes. And please do not start Googling symptoms at 2 a.m. (That road leads to… a lot.)
If it’s a night terror: don’t wrestle the glitch
With night terrors, the instinct is to shake someone awake or restrain them. Usually that’s not helpful and can escalate agitation [AASM ICSD-3-TR, 2023].
What helps most:
- Don’t force wake ups unless there’s immediate danger.
- Keep them safe.
Clear obstacles, block stairs, gently guide away from sharp furniture. Calm voice, minimal stimulation.
Most episodes are short (often minutes), and the person usually has little to no memory afterward [AASM ICSD-3-TR, 2023].
When it’s time to call in professional backup
You don’t get a gold star for suffering through this alone.
Make an appointment if:
For panic attacks:
- episodes are recurring, or you’re starting to fear sleep
- you’re losing significant sleep or avoiding bedtime
- you also have daytime panic/anxiety symptoms
For night terrors:
- they start in adulthood or suddenly get worse [AASM ICSD-3-TR, 2023]
- there’s risky behavior (leaving the bed/house) or injuries
- they’re becoming more frequent
- there’s loud snoring, witnessed pauses, or recurrent gasping (rule out sleep apnea) [AASM Sleep Apnea Overview]
Who do you see?
- Night terror pattern → often sleep medicine (sometimes a sleep study helps rule out sleep apnea or seizures)
- Nocturnal panic pattern → often psychologist/psychiatrist (or primary care to start), especially if there’s broader anxiety
Not sure? Starting with primary care or sleep medicine can be a practical first step when the picture is unclear.
Treatment options (aka: yes, this can get better)
I love “boring sleep” with my whole heart. And yes both of these can improve a lot with the right approach.
- Night terrors:
In kids, they often fade with age. In adults, the focus is usually sleep consistency, stress reduction, and safety. Clinicians also look for triggers like sleep deprivation, alcohol, and untreated sleep apnea [AASM ICSD-3-TR, 2023]. Medication is typically reserved for severe cases (injury risk) and is firmly “doctor territory.” - Nocturnal panic attacks:
These often respond well to treatment. CBT for panic is a frontline option, and medications such as SSRIs may be used when attacks are frequent or impairing (personalized decision with a clinician) [APA DSM-5-TR, 2022].
If you’re seeing a clinician, bring intel
Your future appointment goes smoother if you track:
- when episodes started
- how often they happen
- what time of night
- what you felt/did
- how much you remember
- how long it took to fall back asleep
- alcohol/caffeine/stimulants, and any med changes
A simple two week sleep diary helps. If you have a partner who witnesses episodes, their notes matter. If you can safely capture a video, it can be diagnostically useful don’t risk injury to get it.
The takeaway (tattoo it on your pillow… kidding)
If you remember it vividly, it’s more likely nocturnal panic.
If you have no memory and someone else witnessed the chaos, it’s more likely a night terror [AASM ICSD-3-TR, 2023. APA DSM-5-TR, 2022].
That one “memory check” won’t solve everything but it cuts through a shocking amount of confusion and points you toward the right kind of help.
Frequently Asked Questions
Does the “Do you remember it?” test really work for night terrors vs panic attacks?
It’s a useful first sort because amnesia/confusion is common with night terrors (NREM parasomnias), while clear recall is more typical of panic attacks [AASM ICSD-3-TR, 2023. APA DSM-5-TR, 2022]. It’s not perfect sleep apnea, reflux, seizures, nightmares, and medication effects can blur the picture.
Can panic attacks happen during sleep?
Yes. Some people have panic attacks that occur after falling asleep (nocturnal panic), and they can feel especially alarming because you wake up mid surge [APA DSM-5-TR, 2022]. If episodes are recurrent, treating panic (often CBT and sometimes medication) can make a big difference.
How long do nocturnal panic attacks last?
The most intense part often peaks within minutes, but the “after shock” (shakiness, dread, trouble falling back asleep) can linger longer. If symptoms are persistent/worsening or come with red flags (fainting, severe chest pain, severe shortness of breath), get urgent medical help [American Heart Association Heart Attack Warning Signs].
When should I do the memory test and what should I write down?
Do it as soon as you’re steady enough to note: time, what you remember, breathing symptoms, what your body did, and how long until you fell back asleep. A two week log is often enough to spot patterns worth bringing to a clinician.
Are there risks to “just assuming it’s panic” if I’m waking up choking or gasping?
Yes because recurrent gasping can signal obstructive sleep apnea or, in some cases, reflux related laryngospasm [AASM Sleep Apnea Overview. Cleveland Clinic Laryngospasm]. If choking/gasping is a main feature, especially with snoring or daytime sleepiness, get evaluated rather than self labeling.
Is a night terror the same as a nightmare?
Not usually. Night terrors are typically NREM parasomnias with confusion and limited recall, while nightmares are more often REM related with clearer dream memory [AASM ICSD-3-TR, 2023]. If you’re acting out dreams (kicking/punching), ask about REM sleep behavior disorder [Mayo Clinic REM Sleep Behavior Disorder].
When should I see a doctor about this?
See a healthcare provider if episodes happen weekly, you’re injuring yourself/others, you regularly wake gasping/choking, you have daytime sleepiness that affects safety, or sleep problems persist more than ~3 weeks and impair your functioning. Seek urgent care right away for chest pain with concerning features, fainting, new neurologic symptoms, or seizure like activity [American Heart Association Heart Attack Warning Signs. NINDS Seizures Overview].
Last updated: 2025-12-23
Sources
- American Academy of Sleep Medicine (AASM). International Classification of Sleep Disorders, Third Edition Text Revision (ICSD-3-TR). 2023. (clinical reference)
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed., Text Revision (DSM-5-TR). 2022. (clinical reference)
- American Heart Association. “Heart Attack Symptoms.” https://www.heart.org/ (overview)
- American Academy of Sleep Medicine (AASM). “Sleep Apnea.” https://sleepeducation.org/sleep-disorders/sleep-apnea/ (overview)
- National Institute of Neurological Disorders and Stroke (NINDS). “Seizures and Epilepsy.” https://www.ninds.nih.gov/health-information/disorders/seizures-and-epilepsy (overview)
- Cleveland Clinic. “Laryngospasm.” https://my.clevelandclinic.org/health/diseases/22406-laryngospasm (overview)
- Mayo Clinic. “REM sleep behavior disorder.” https://www.mayoclinic.org/ (overview)