The 2 A.M. test every parent needs
There are few sounds more adrenaline inducing than a child screaming in the dark. It’s like your nervous system gets yanked out of bed before your body even catches up. One second you’re asleep, the next you’re sprinting down the hallway in full panic… directly onto a Lego (because of course).
The short answer: If your child remembers what happened, it’s usually a nightmare. If they don’t remember anything the next day, it’s more likely a night terror.
Key exception: If episodes involve breathing trouble, injury, seizure like movements, or prolonged confusion, treat it as a medical concern not “just sleep stuff.”
When it matters less: If episodes are rare and your child is otherwise healthy and well rested, both nightmares and night terrors are common in childhood and often improve with time [AAP HealthyChildren.org, NHS].
Last updated: 2025-12-23. This is educational content and isn’t a substitute for care from your child’s pediatrician.
So first: you’re not alone, and you’re not “doing bedtime wrong.” Nightmares happen to basically everyone at some point, and night terrors are fairly common in kids with prevalence estimates varying a lot by age and definition (some studies report up to ~30% having at least one episode, while frequent/recurrent terrors are less common) [AAP HealthyChildren.org, ICSD-3].
Let’s make it simple. Because you deserve a simple.
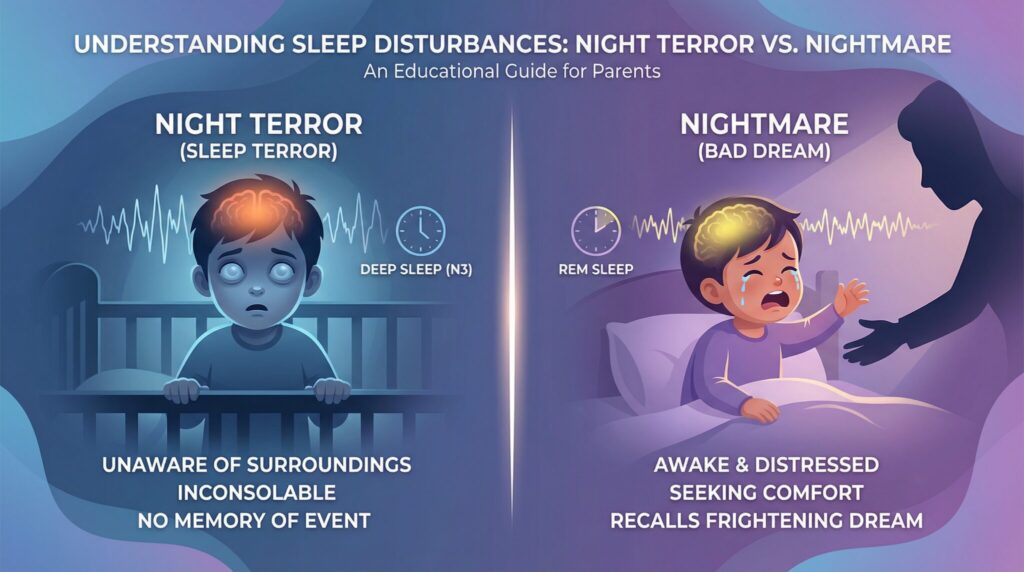
Quick comparison: night terror vs nightmare
| Clue | Night terror (NREM parasomnia) | Nightmare (REM dream) | What you do |
|—|—|—|—|
| When it happens | Often first third of the night (more deep sleep early) [ICSD-3] | More often later in the night / early morning (more REM later) [Mayo Clinic] | Use timing as a hint not a guarantee |
| Do they “wake up”? | Not fully. Can look awake but brain isn’t fully online | Yes. Fully awake and seeking reassurance | Terror: protect + wait it out. Nightmare: comfort + reassure |
| Do they recognize you? | Often no (blank stare, confused) | Usually yes | Recognition is a huge clue |
| Morning memory | Typically no recall | Often some recall (even if fuzzy) | Ask in the morning don’t interrogate at 2 A.M. |
| How it ends | Often ends abruptly. Child settles back down | Needs comfort. May fear returning to sleep | Different “parent job” |
| Typical length | Usually a few minutes, sometimes longer. If consistently prolonged, get help [NHS, Mayo Clinic] | Variable | Track duration either way |
The Quickest Way to Tell: The Morning-After Memory Test
Here’s my cheat code, and it works shockingly well:
If they remember it, it was probably a nightmare. If they don’t remember a thing, it was probably a night terror.
That’s it. That’s the magic trick.
- Nightmares happen in REM sleep (dream sleep). Your kid wakes up and can often tell you what happened: the giant spider, the “bad guy,” the falling off a cliff thing [Mayo Clinic].
- Night terrors happen out of deep non-REM sleep (a NREM parasomnia). Their body can look like it’s in full meltdown mode (screaming, sweating, racing heart), but their brain isn’t fully “awake” in the way you expect [ICSD-3]. In the morning? Often no memory.
Parenthood is truly just you collecting intense memories on behalf of someone else.
Second Clue: What Time It Happens (AKA Your Clock Is Smarter Than You at 2 A.M.)
Timing isn’t perfect, but it’s a really helpful hint:
- Night terrors: often in the first 1-3 hours after they fall asleep (when deep sleep is most concentrated) [ICSD-3].
- Nightmares: more likely in the last third of the night (more REM toward morning) [Mayo Clinic].
So if your kiddo is screaming at 10:30 p.m. and seems not really reachable… that leans “night terror.” If they wake up near morning and immediately start telling you about the scary dog with human teeth… that’s a nightmare.
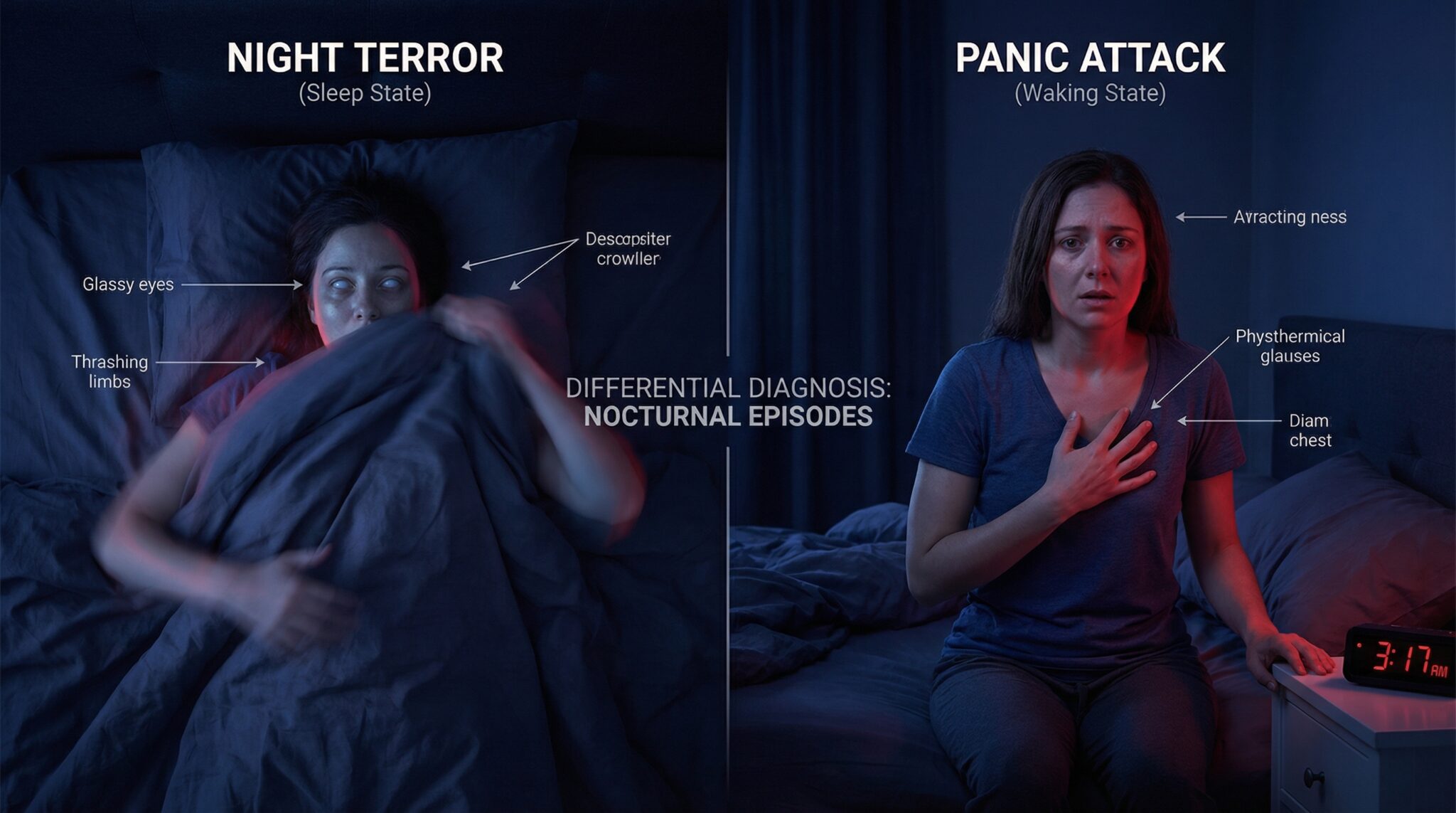
What You’ll See In the Moment (Because You Don’t Have Time for a TED Talk)
When you step into the room, look for these two real world clues:
1) Do they recognize you?
- Nightmare: they know you, they want you, they can usually answer you.
- Night terror: their eyes might be open, but it’s like they’re looking through you.
2) How does it end?
- Nightmare: they usually need comfort to settle back down.
- Night terror: it often ends abruptly and they fall back to sleep.
Pocket mantra: Timing + memory beats panic every time.
So… What Exactly Is a Night Terror?
Night terrors are the horror movie version of sleep except your kid is not actually “watching” the movie.
During a night terror, they might sit up, scream, thrash, sweat, breathe fast, even get out of bed. They may not respond to you, and too much interaction can sometimes escalate the confusion [NHS]. Episodes are often short (a few minutes), but can be longer. If they’re consistently prolonged or getting dangerous, that’s a reason to get medical guidance [NHS, Mayo Clinic].
The weirdest comfort: night terrors usually look worse to you than they feel to them. They aren’t fully conscious the way they are in a nightmare, and they typically won’t remember it in the morning [AAP HealthyChildren.org].
Night terrors are most common in early childhood, often around preschool/early school age, and many kids improve as sleep matures [AAP HealthyChildren.org]. If an adult suddenly starts having them or a child’s episodes come with major red flags get checked out.
And a Nightmare?
Nightmares are the ones that feel personal like your kid’s brain wrote a scary screenplay and cast them as the lead.
With a nightmare, your child wakes up and can usually talk right away. They know where they are. They know who you are. They’re upset because the dream felt real, and now they need help climbing out of it.
This is where you’re less “silent safety guardrail” and more “cozy reality check person.” Different job. Same pajamas.
Common Triggers (No, It’s Not Always That One Episode of a Kids’ Show)
Triggers aren’t blame. They’re clues.
Night terrors are often about disrupted sleep (and a nervous system that’s overtired). Think:
- not enough sleep (big one)
- inconsistent bedtime/wake time
- fever/illness
- full bladder
- the nap to no nap transition
Nightmares are often about big feelings + an active brain. Think:
- stress/anxiety
- trauma/PTSD
- certain medications (for example, some medications that affect sleep architecture ask your clinician/pharmacist if you suspect a link)
- scary content too close to bedtime
- fatigue (sometimes once they finally get REM sleep, dreams get intense)
One more nerdy but useful note: nightmares about drowning or suffocating can sometimes be nightmares that hint at health issues and show up alongside sleep disordered breathing (like obstructive sleep apnea), because the brain may weave physical sensations into dreams. It’s not the most common explanation, but if you also notice loud snoring, gasping, or breathing pauses, bring it up with your pediatrician [AAP OSA Guideline].
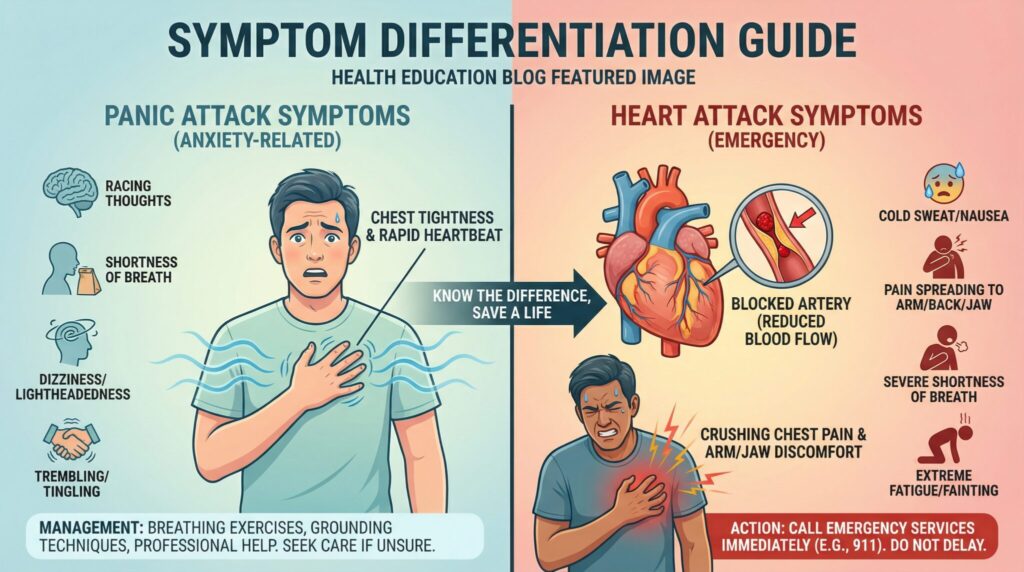
Could it be something else? (Look-alikes worth knowing)
Because yes sometimes it’s neither.
- Confusional arousals: a cousin of night terrors (partial waking from deep sleep) where kids may cry, be disoriented, and resist comfort, with little/no memory later [ICSD-3].
- Sleepwalking: can overlap with night terrors. Safety proofing matters if your child is wandering [ICSD-3].
- Nocturnal seizures: can mimic parasomnias. Red flags include rhythmic jerking, stiffening, episodes that look very similar each time, tongue biting, incontinence, or confusion that lasts longer than expected afterward [NHS].
- Panic symptoms: older kids/teens may wake with panic like symptoms and full awareness (more consistent with nightmares/anxiety than night terrors).
- Reflux/GERD: some kids wake distressed, coughing, or choking. If you see frequent nighttime cough, sour breath, or pain, talk to your clinician.
- Medication/substance effects: stimulants, some antidepressants, antihistamines, and melatonin timing/dose issues can all change sleep in some kids worth reviewing with a clinician if episodes started after a change.
What to Do at 2 A.M. (The Part You Actually Came For)
If It’s a Night Terror: Usually Don’t “Fully” Wake Them
I know. It feels wrong. They look so upset. Your instincts are screaming, “WAKE UP MY BABY!”
But trying to force a full awakening during a night terror can make things worse for some kids more confusion, longer episode, louder screaming [NHS]. (Key word: force. Safety comes first.)
Instead:
- Stay close and keep them safe (think: human guardrail)
- Don’t restrain them unless they’re about to get hurt
- Move obstacles away if they’re flailing or trying to walk
- If you talk, keep it low and calm
- Let it pass
- Gently guide them back to bed if needed
Also: don’t make it a big “talk” in the morning unless they bring it up. If they don’t remember, replaying it in detail can sometimes plant bedtime anxiety.
If your child is a mover (sleepwalking overlap): consider practical safety steps like a baby gate at stairs, clearing floor clutter, and securing exterior doors/windows.
If It’s a Nightmare: Comfort Works (Bring the Snuggles)
With nightmares, your kid is awake enough to receive comfort so give it.
My go to steps:
- Make eye contact, use their name, keep your voice calm
- Remind them: “You’re safe. You’re in your room. That was a dream.”
- Offer a hug/hand squeeze/water (whatever helps your kid)
- If talking about details winds them up, don’t dig. You can chat about it in daylight.
- Use simple grounding: “Can you tell me three things you see in your room?”
Comfort first, detective work later.
Preventing More of This (AKA The Boring Stuff That Works)
Yes, prevention is unglamorous like flossing, but for sleep. Still: it’s the heavy hitter.
If you do nothing else, aim for:
- a consistent bedtime and wake time (even weekends… I’m sorry)
- enough total sleep (for many kids: 10-13 hours for ages 3-5, and 9-12 hours for ages 6-12) [AASM Sleep Duration Consensus]
- a cool, dark room
- screens off at least an hour before bed (especially for kids who get “revved up” easily)
You don’t need a $200 star projector that looks like a galaxy threw up in your child’s room. Consistency is the thing.
If Night Terrors Are Predictable: Try Scheduled Awakenings
If the night terrors happen like clockwork (rude), this can help for some families:
- Track the usual time for about a week
- Wake your child gently 15-30 minutes before that time
- Keep them awake for a minute or two, then let them go back to sleep
- Try it for 2-4 weeks
The idea is to interrupt the deep sleep pattern where these episodes tend to pop up [Mindell & Owens, Clinical Guide to Pediatric Sleep].
If Nightmares Are Frequent: Work on the Day, Not Just the Night
Because the best bedtime routine in the world can’t outsmart a day that felt too big.
- Talk about worries earlier in the day (not right before lights out)
- Cut scary content, especially close to bedtime
- For frequent, intense nightmares, Imagery Rehearsal Therapy (IRT) can help some people (rewriting the dream while awake and practicing the new version). Evidence is strongest in adolescents/adults, but clinicians sometimes adapt it for kids too [Aurora et al., 2010].
When to Call the Doctor (Because Sometimes You Need Backup)
If your gut says, “This isn’t just a quirky phase,” listen to it and notice signs to talk to a clinician.
Call for urgent help now (ER/911/local emergency number) if:
- your child has trouble breathing, turns blue/gray, or you see prolonged breathing pauses
- there’s a serious injury, or they can’t be kept safe
- you suspect poisoning/ingestion
- the episode includes seizure like activity (rhythmic jerking, stiffening) or your child has prolonged confusion afterward
- the event lasts a long time and your child isn’t returning toward baseline
Check in soon about night terrors if:
- they’re happening more than 2-3 times a week consistently
- they’re often lasting >10-15 minutes
- your child is getting hurt or wandering unsafely
- they continue well into adolescence
- they start for the first time in adolescence/adulthood
Get help for nightmares if:
- they’re weekly (or more) and disrupting life
- your child becomes afraid of sleep or bedtime becomes a daily battle
- the same nightmare repeats over and over
- they started after trauma or come with other PTSD symptoms
- you’re seeing major mood/anxiety changes
Getting support isn’t a failure. It’s a strategy.
If you do see a clinician: what to track (this helps a lot)
If you’re heading toward a pediatrician visit (or a sleep specialist), a little data makes the appointment way more useful:
- time they fell asleep + how long after sleep onset the episode happened
- how long it lasted (best guess)
- what you saw: sitting up, walking, sweating, thrashing, talking, screaming
- responsiveness: did they recognize you, could they answer questions
- recent sleep loss, illness/fever, new stress, new meds/supplements
- snoring, gasping, mouth breathing, restless sleep (possible sleep disordered breathing) [AAP OSA Guideline]
- video (only if safe and you can do it without delaying care)
Frequently Asked Questions
How can I quickly tell night terrors vs nightmares?
Use the trio: timing + recognition + morning memory. Early night + “not reachable” + no memory points to night terrors. Later night + clearly awake + remembers points to nightmares [ICSD-3, Mayo Clinic].
Should I wake my child during a night terror?
Usually, it’s better not to force a full awakening, because it can prolong or intensify the episode for some kids [NHS]. Focus on safety and calm presence. If there’s danger (wandering, injury risk), it’s okay to turn on lights and gently orient them safety beats “rules.”
How long do night terrors last?
Many episodes last a few minutes, but some last longer. Consistent episodes >10-15 minutes, very frequent episodes, or unsafe wandering are reasons to ask for medical guidance [NHS, Mayo Clinic].
Are frequent nightmares a sign of anxiety or trauma?
They can be. Nightmares often cluster during stress, anxiety, and after scary experiences. If they started after trauma or come with daytime symptoms (avoidance, hypervigilance, mood changes), it’s worth discussing with a clinician or therapist.
What if my child has reflux, snores, or takes medications?
Reflux can disrupt sleep and cause distress. Snoring/gasping can signal sleep disordered breathing, which deserves evaluation [AAP OSA Guideline]. If episodes began after starting or changing a medication (or supplement like melatonin), ask your pediatrician or pharmacist about sleep side effects and safer timing.
Is food/sleep hygiene enough, or do we need therapy?
Many kids improve with sleep consistency and enough total sleep [AASM Sleep Duration Consensus]. If nightmares are persistent, distressing, or trauma linked, therapies like Imagery Rehearsal Therapy may help (often with professional guidance) [Aurora et al., 2010].
When should I see a doctor about this?
Make an appointment if episodes are frequent, dangerous, prolonged, tied to snoring/gasping, or causing daytime impairment or if your child becomes afraid of sleep. Seek urgent care for breathing problems, significant injury, suspected ingestion, or seizure like activity.
Your “What Just Happened?” Nighttime Plan
If you’re standing in the hallway tonight with your heart pounding, here’s what to remember:
1) What time is it? (early night = terror, late night = nightmare)
2) Do they recognize you? (yes = nightmare, no = terror)
3) In the morning, do they remember? (yes = nightmare, no = terror)
Then respond accordingly: terrors = safety and let it pass, nightmares = comfort and reassurance.
And if nothing else, know this: both are common, both are survivable, and you’re not alone just temporarily employed as the nighttime security system.
Sources
- American Academy of Pediatrics (AAP). “Nightmares and Night Terrors.” HealthyChildren.org. (overview) https://www.healthychildren.org
- NHS. “Night terrors.” National Health Service. (overview) https://www.nhs.uk
- American Academy of Sleep Medicine. International Classification of Sleep Disorders (ICSD-3). AASM, 2014. (clinical reference)
- Mayo Clinic Staff. “Night terrors (sleep terrors).” Mayo Clinic. (overview) https://www.mayoclinic.org
- Paruthi S, Brooks LJ, D’Ambrosio C, et al. “Recommended Amount of Sleep for Pediatric Populations.” Journal of Clinical Sleep Medicine, 2016. (consensus statement)
- Marcus CL, Brooks LJ, Ward SD, et al. “Diagnosis and Management of Childhood Obstructive Sleep Apnea Syndrome.” Pediatrics, 2012. (guideline)
- Mindell JA, Owens JA. A Clinical Guide to Pediatric Sleep: Diagnosis and Management of Sleep Problems. (clinical reference/book)
- Aurora RN, Zak RS, Auerbach SH, et al. “Best practice guide for the treatment of nightmare disorder in adults.” Journal of Clinical Sleep Medicine, 2010. (guideline/review)