If your dreams recently went from “mildly odd” to “why am I being chased through an IKEA by a flaming spreadsheet,” you’re not imagining things. Certain medications can crank up vivid dreams and nightmaresespecially right after you start them or when your dose changes.
The short answer: Yessome medications (and some medication changes/withdrawals) can trigger vivid dreams or nightmares, and many cases improve with timing tweaks, slower dose changes, within-class switches, and evidence-based nightmare therapy.
Key exception: If you’re acting out dreams, having hallucinations/confusion, or the nightmares involve self-harm thoughts, treat it as urgent and contact a clinician (or emergency help) right away.
When it matters less: If the dreams are vivid but you’re safe, functioning, and they started right after a new med/dose change, this is often fixable with supervised adjustmentsno need to panic.
And yes, it’s wildly unfair that you can finally get your blood pressure/mood/sleep/whatever under control… and then your brain decides to screen a horror festival at 3:47 a.m.
The good news: a lot of med-related nightmare issues improve with pretty simple adjustments (timing, slower changes, switching within the same medication family, or adding a specific therapy). The most important news: there’s one safety rule you don’t get to skip.
The one rule: don’t DIY your meds (I’m begging you)
I’m going to be the boring mom-friend for a second because boring is how we keep you safe:
Don’t stop, skip, or change doses on your own.
This is especially true for antidepressants, beta blockers, sleep meds/benzos, Parkinson’s medications, seizure medications, and steroids. Abrupt changes can trigger rebound symptoms and withdrawal effectsand in some situations can be dangerous (blood pressure spikes, severe withdrawal, agitation, neurologic symptoms, seizures). (If you’re on multiple meds, the safest path is usually a supervised plannot a rage-quit.)
If the nightmares are making you miserable, that’s real. But your dreams don’t get to bully you into unsafe medication changes.
When nightmares are a “call someone now” situation
Most nightmare stuff is “make an appointment soon” territory. But get urgent help if you have any of these:
- You’re acting out dreams (punching/kicking/falling out of bed) and could hurt yourself or a partner (this can fit REM sleep behavior disorder) [AASM, 2014].
- Nightmares come with confusion, hallucinations, memory problems, or you feel persistently “not right” when you wake up
- Dream content includes self-harm/suicidal thoughts, or you wake up with those thoughts lingering
- You’re so scared of sleeping that you’re avoiding it (or you’re becoming unsafe to drive/work because you’re exhausted)
Those can point to issues that need prompt medical attention (sometimes a sleep study, sometimes med changes, sometimes both).
If you’re having thoughts of harming yourself or you feel like you might act on them, seek emergency help now. In the U.S., you can call/text 988 (Suicide & Crisis Lifeline). If you’re outside the U.S., use your local emergency number or crisis line.
How to tell if your medication is the culprit (vs. life being… life)
A super common pattern with medication-related nightmares is:
- They start within days to about 4 weeks of starting a medication or increasing a dose (varies by drug and person)
- They happen often (nightly or close to it)
- They’re more common in the second half of the night (hello, 4 a.m. dread), when REM sleep naturally stacks up
If you’ve been on the same meds for years and the nightmares start out of nowhere, it might still be medication-related, but it’s often more likely something else is piling onstress, trauma, sleep deprivation, sleep apnea, new substances/supplements, or a new medical issue.
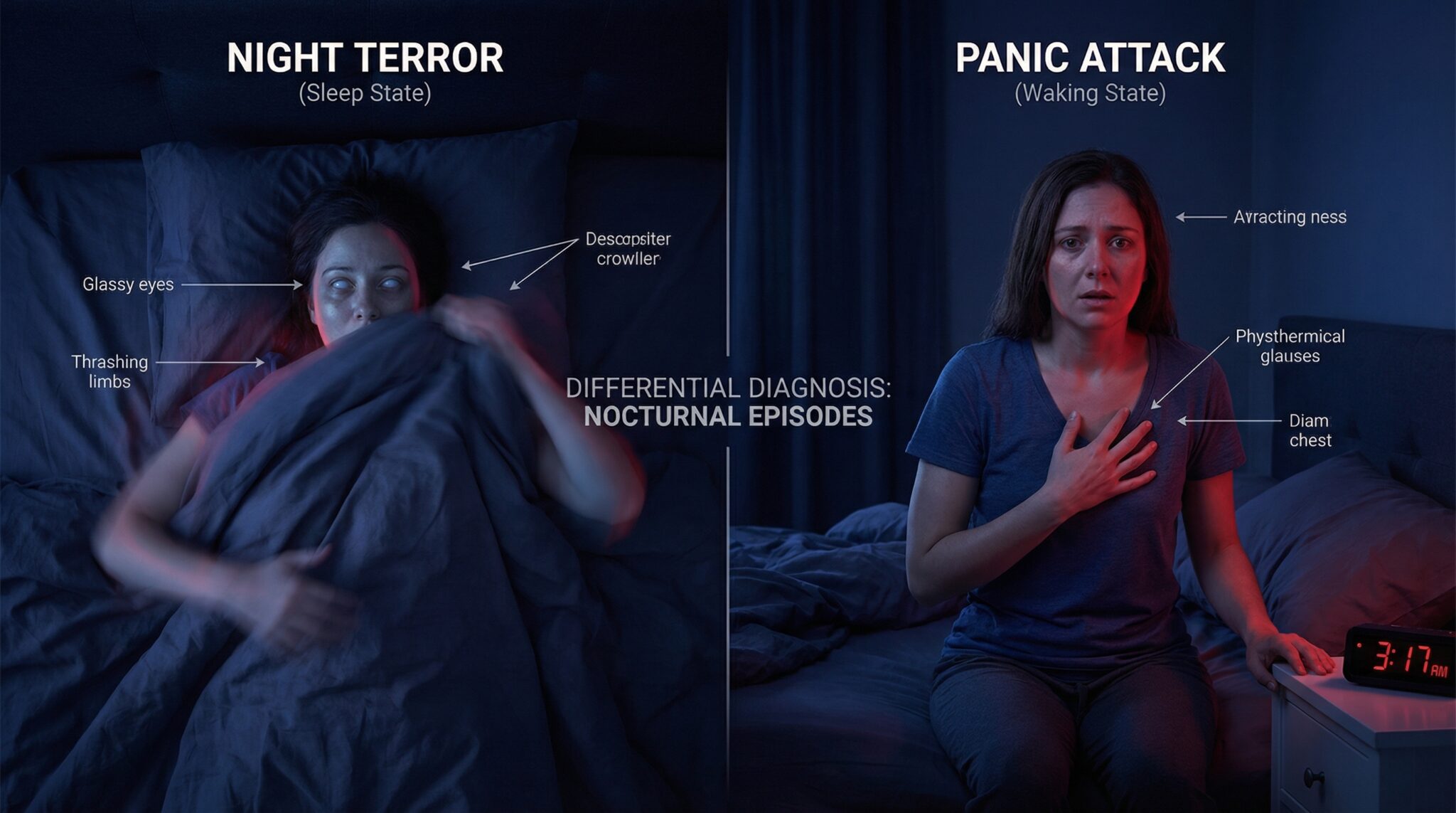
Also worth knowing: acting out dreams with little/no recall can be a different issue (REM behavior disorder) and is worth flagging to a clinician promptly [AASM, 2014].
Quick clarity: vivid dreams vs. nightmares vs. night terrors (and why meds can change them)
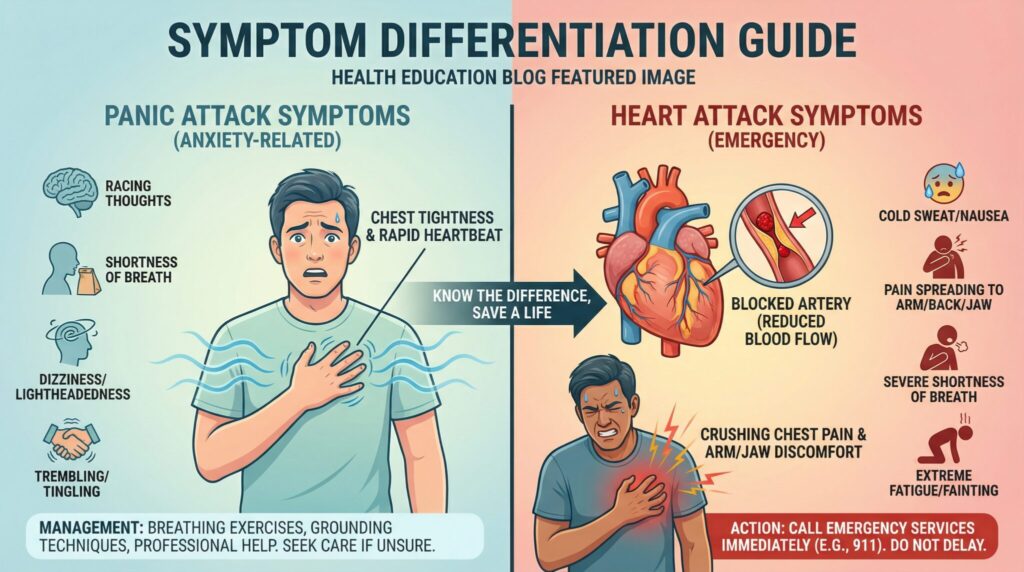
These get lumped together online, but they’re not the same:
- Vivid dreams: intense, detailed dreams, not always distressing.
- Nightmares: disturbing dreams that usually wake you up and leave you upset/alert.
- Night terrors: typically early-night episodes (more common in kids) with screaming/panic and limited recall.
- REM sleep behavior disorder (RBD): you physically act out dreams because the normal REM “paralysis” is impairedthis is a safety issue and needs medical evaluation [AASM, 2014].
Why medications can mess with dreams (the short version):
- Some meds change REM sleep (how much you get, how intense it is, or how “dense” it feels) [Wilson & Argyropoulos, 2005].
- Some meds fragment sleep or increase awakenings. The more you wake up during/after REM, the more likely you are to remember dreamssometimes as “more nightmares,” even if REM didn’t increase.
- Stopping certain REM-suppressing meds too quickly can contribute to REM rebound (a temporary surge in REM/dream intensity) [Wilson & Argyropoulos, 2005].
Do this first: keep a tiny “sleep receipts” log for 1-2 weeks
You do not need a perfect spreadsheet. You need “good enough” notes you can hand to your prescriber so they don’t have to play Guess Who: Nightmare Edition.
Write down:
- Medication name + dose + time you took it
- Nightmare intensity (1-10) (1 = mildly annoying, 10 = I need to sage the bedroom)
- When it happened (early night vs. toward morning)
- Overall sleep quality (separate from the dreambecause sometimes you sleep deeply and still have terrifying dreams)
- Any recent changes (new med, dose increase, quitting something, added supplements like melatonin, nicotine patch, cannabis, alcohol)
Patterns show up faster than you’d think. And walking into an appointment with “This started 10 days after my dose change and happens mostly when I take it at night” is chef’s kiss helpful.
Medications that can cause nightmares: a scannable cheat sheet
Not everyone gets nightmares from these. This is a “common enough to be worth checking” listespecially when timing lines up.
| Medication/class | Examples (not exhaustive) | How soon it can show up | Evidence strength* | What to ask your prescriber |
|—|—|—:|—|—|
| SSRIs/SNRIs | sertraline, fluoxetine, venlafaxine, duloxetine | daysweeks | Promising/known sleep-effects [Wilson & Argyropoulos, 2005] | “Can we adjust timing or titration speed?” |
| Other antidepressants | bupropion, mirtazapine, TCAs/MAOIs | daysweeks | Mixed (varies by agent) [Thompson & Pierce, 1999] | “Is this a known side effect for this one?” |
| Beta-blockers | propranolol, metoprolol (varies) | daysweeks | Mixed [Thompson & Pierce, 1999] | “Could we change timing or try a different option?” |
| Cholinesterase inhibitors | donepezil, rivastigmine, galantamine | daysweeks | Known (label-listed) [FDA Donepezil PI] | “Would morning dosing reduce vivid dreams?” |
| Parkinson’s / dopaminergic meds | carbidopa/levodopa, pramipexole, ropinirole | daysweeks | Mixed/known in practice | “Which one is most likely? Can we adjust slowly?” |
| Stimulants / ADHD meds | methylphenidate, amphetamines | days | Mixed | “Is the dose too late in the day?” |
| Antiseizure meds | topiramate, levetiracetam | daysweeks | Mixed | “Could this be a CNS side effect vs sleep disruption?” |
| Antimalarials | mefloquine | daysweeks | Well-established neuropsychiatric risk [FDA Mefloquine Safety] | “Is there a safer alternative for me?” |
| Smoking cessation | varenicline, nicotine patch | days | Known (label-listed for varenicline) [FDA Varenicline PI] | “Can we adjust dose/timing or change strategy?” |
| Steroids | prednisone | often quickly | Common sleep disturbance | “Can I take it earlier? Is taper needed?” |
| Sleep “helpers” (OTC) | diphenhydramine, doxylamine | days | Mixed, common complaint | “What’s a better long term plan than OTC sedatives?” |
*Evidence strength here reflects a mix of clinical reviews, prescribing info, and consistent patient reportsnot a guarantee you’ll experience it.
The “usual suspects” (aka: meds that commonly mess with dreams)
I’m not saying these meds are bad. I’m saying your brain can be dramatic about them.
1) Beta-blockers (blood pressure/heart rate meds)
These are frequent flyers in nightmare land for some peopleespecially certain beta-blockerswith dream disturbances described in clinical reviews and case reports [Thompson & Pierce, 1999].
What to ask your prescriber:
- “Could timing help?” (taking it earlier sometimes shifts the nightmare windowbut don’t change timing if your clinician is using it for a specific blood pressure/heart rhythm goal)
- “Is there a comparable option that’s less likely to cause CNS side effects for me?” (this varies by your condition and the specific beta-blocker)
Also: don’t panic if you need a beta-blocker. The goal is treated and well-rested, not “pick one.”
If you have asthma/COPD or very low blood pressure: timing or drug changes matter more and should be clinician-guided.
2) Antidepressants (SSRIs/SNRIs—and a few others)
SSRIs/SNRIs can change REM sleep, dream intensity, and dream recall in some people [Wilson & Argyropoulos, 2005]. The timing can be annoyingly specific: sometimes it ramps up after the first couple weeks, right when you’re thinking, “Hey, I might be feeling better,” and then your dreams go full gothic novel.
A very common, very simple tweak to ask about:
- Morning dosing (when appropriate for your specific medication and symptoms) may help some people.
And a huge note in bold: stopping antidepressants can temporarily make dreams worse, especially with abrupt changes (REM rebound/withdrawal effects can be part of that) [Wilson & Argyropoulos, 2005]. If you’re tempted to quit because of nightmares, please bring it up insteadthere are safer ways to adjust.
Other antidepressants that come up a lot in “wild dreams” stories:
- Bupropion, mirtazapine, and sometimes TCAs/MAOIs (varies widely by person and agent) [Thompson & Pierce, 1999].
If you have bipolar disorder or a history of mania/psychosis: any antidepressant change should be handled carefully and promptly with your prescriber.
3) Statins (cholesterol meds)
Statins don’t cause nightmares for everyone (or even most people), but some people do report a clear connection. The evidence is mixed, and it’s not always easy to separate dream effects from sleep disruption in general (or from unrelated stressors) [Thompson & Pierce, 1999].
What to ask about:
- “If this timing fits, could we try a different statin or dosing time and see if it changes?”
(Any change should weigh cholesterol benefits vs. sleep side effects for you.)
4) “Sleep helpers” that… don’t help
The irony is strong here. Some sleep medicationsand especially older OTC antihistaminescan make sleep feel weird and fragmented, or make dream recall more intense.
Common culprits:
- Diphenhydramine (Benadryl / ZzzQuil / Tylenol PM) and doxylamine (Unisom)
Also: melatonin isn’t automatically the gentle angel everyone thinks it is. Dose, timing, and product quality vary, and some people feel worse (more vivid dreams, next-day grogginess, fragmented sleep). If you’re taking melatonin alongside other sedating meds or antidepressants, it’s worth mentioning in your log.
What to ask about:
- “Is there a non-med option that would actually fix the sleep issue?” (CBT-I is first-line for chronic insomnia) [Qaseem et al., 2016]
- “Is there a lower-risk alternative for allergies/sleep in my situation?” (Often yesbut it depends on your health conditions and other meds.)
If you’re pregnant or trying to conceive: ask before using sleep supplements (including melatonin), because safety data and regulation vary.
5) Parkinson’s medications (and dopamine-related meds)
If you or a loved one is dealing with Parkinson’s, vivid dreams can be a real part of the picturesometimes from the condition itself, sometimes from dopamine-related meds (and often from a mix).
Examples people often ask about:
- Carbidopa/levodopa
- Dopamine agonists like pramipexole or ropinirole
What to ask about:
- “Which med in the mix is most likely to be doing this?”
- “Could we adjust timing or dose changes more slowly?”
This is absolutely not a category to freestyle. It’s a “small tweaks, carefully supervised” situation.
6) Dementia meds that can supercharge dreams (cholinesterase inhibitors)
This one catches families off guard: donepezil (and similar meds) can cause abnormal dreams/nightmares, and it’s listed in prescribing information [FDA Donepezil PI].
What to ask about:
- “Would switching to morning dosing help?” (This is a common clinician movebut do it with guidance.)
If falls are a risk (older adults, balance issues): vivid dreams + nighttime confusion + getting out of bed can be a dangerous combobring it up quickly.
Bonus round: other high-signal offenders (including withdrawals)
A few other meds/substances that commonly show up in nightmare stories include:
- Varenicline (Chantix) (abnormal/vivid dreams are label-listed) [FDA Varenicline PI]
- Nicotine patch (some people do better removing it at nightask first, because it can affect cravings/quit success)
- Prednisone and other steroids (often improves when the course ends or when taken earlier)
- Antiseizure meds like topiramate or levetiracetam (some people report vivid dreams/mood effects)
- Stimulants (especially if taken too late)
- Mefloquine (antimalarial with well-established neuropsychiatric side effects, discuss alternatives if you’re prescribed it) [FDA Mefloquine Safety]
- Opioids, alcohol, cannabis: both use and withdrawal can disrupt sleep architecture and trigger intense dreaming for some people
If your timing lines up, put it in the log. Even if it feels “too random,” your notes help connect dots.
What usually helps (the practical, non-mystical part)
When someone tells me, “My doctor is going to think I’m ridiculous,” I want to grab them gently by the shoulders and say: doctors hear this a lot. Nightmares can be a side effect, not a personality flaw.
Here are the most common fixes to discussstarting with the easiest:
A simple step-by-step “fix it” plan (with what’s safe vs. supervised)
1) Check the timeline (safe to do today)
Look for: new meds, dose increases, missed doses, tapers, quitting substances (alcohol/cannabis/nicotine), new supplements.
2) Screen for red flags (safe to do today)
Acting out dreams, hallucinations/confusion, suicidal thoughts, new neurologic symptoms = urgent evaluation [AASM, 2014].
3) Rule out common non-med drivers (safe to start, evaluation may be needed)
Sleep deprivation, stress/trauma flare, sleep apnea, and restless sleep can all fuel nightmares or dream recall. If you snore loudly, wake gasping, or have major daytime sleepiness, ask about sleep apnea testing.
4) Try “low-risk” adjustmentsONLY if your prescriber agrees (supervised)
- Timing changes (earlier dosing, morning dosing when appropriate)
- Slower titration (smaller steps, longer intervals)
- Within-class switch (e.g., trying a different antidepressant, beta-blocker, statin, etc., based on your medical needs)
5) Add evidence-based therapy for nightmares (safe and effective)
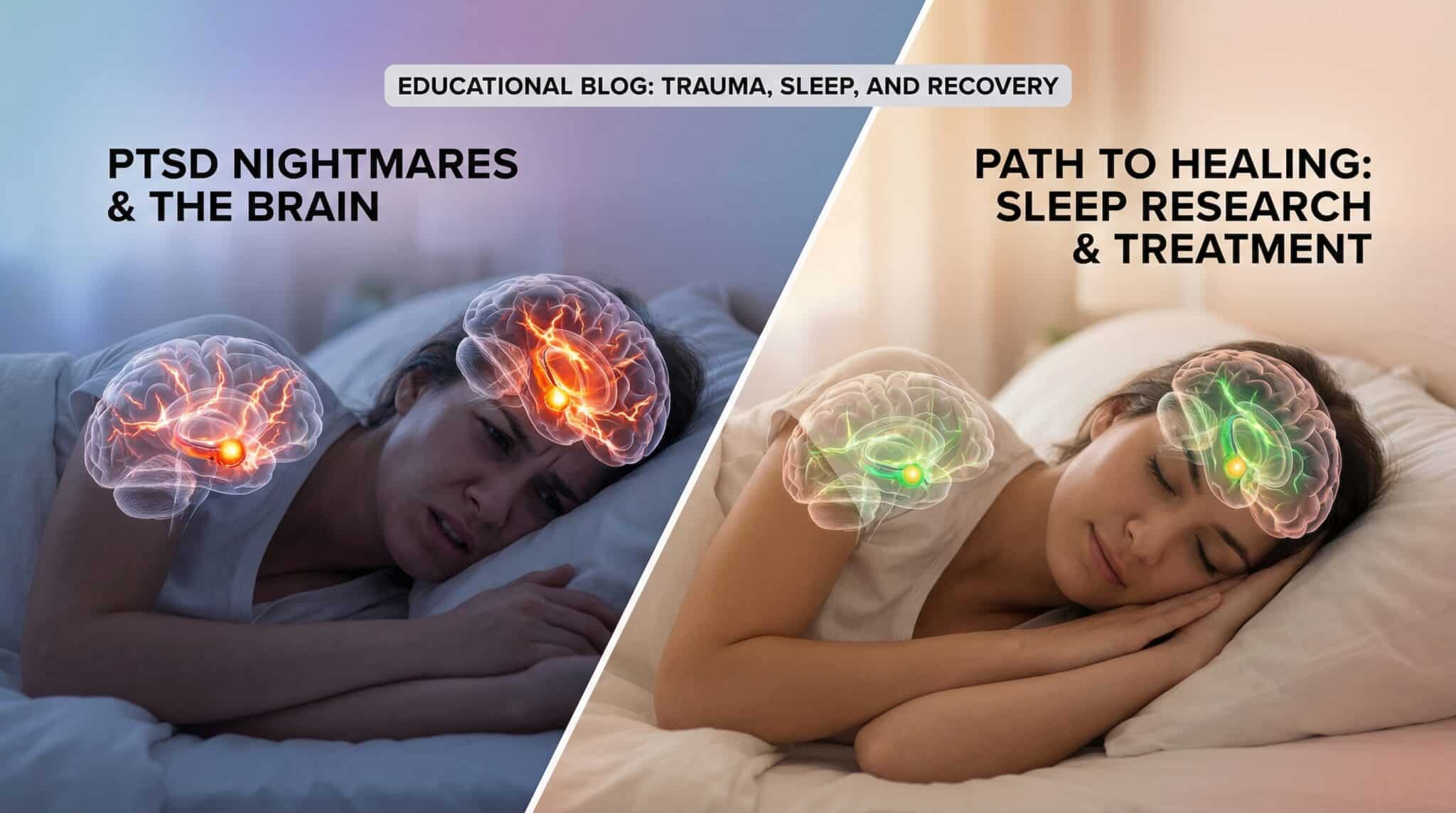
- Imagery Rehearsal Therapy (IRT) has solid evidence for recurrent nightmares, including nightmare disorder and PTSD-related nightmares [Aurora et al., 2010].
- CBT-I helps when insomnia + nightmare anxiety are feeding each other [Qaseem et al., 2016].
6) Consider add-on meds only when there’s a clear “fit” (supervised, risk/benefit)
- Prazosin is commonly used for PTSD-related nightmares, with mixed results across trials and guidelineshelpful for some, not all. It can lower blood pressure and cause dizziness/fainting risk [Aurora et al., 2010, VA/DoD, 2023, Raskind et al., 2018].
- Trazodone is sometimes used for insomnia and may improve sleep for some people, but it’s not a nightmare-specific fix and comes with its own side effects and interaction considerations.
If you have low blood pressure, frequent falls, are on multiple BP meds, or are pregnant: add-on meds require extra caution and individualized guidance.
What to say at your appointment (steal this script)
“I started having vivid dreams/nightmares after starting [med] / increasing to [dose]. It happens [how often], usually [time of night]. I tracked it for [1-2 weeks], and here’s what I noticed. I want to keep treating [condition], but the dreams are affecting my sleep and quality of life. What are our optionstiming, slower changes, switching, or a therapy like IRT/CBT-I?”
That’s it. Calm, specific, and hard to ignore.
Frequently Asked Questions
Which medications commonly cause nightmares or vivid dreams?
Antidepressants (SSRIs/SNRIs and some others), beta-blockers, varenicline, nicotine replacement, steroids, some Parkinson’s meds, donepezil, certain antiseizure meds, stimulants, and mefloquine are frequent “suspects.” Not everyone is affected, so the most useful clue is timing: symptoms that start after a new med or dose change.
How long do medication nightmares last after starting or changing a dose?
Many people notice improvement over days to a few weeks as the body adjusts, but it depends on the medication, dose, and your sleep health. If nightmares are persistent, severe, or worsening after the first few weeks, that’s a good reason to contact your prescriber with your log.
When should I take my medication to avoid nightmaresmorning or night?
For some meds (including some antidepressants and donepezil), morning dosing may reduce vivid dreams for some peoplebut it’s not universal and can backfire for others (e.g., increased daytime side effects). Ask your prescriber before changing timing because it can affect symptom control and side effects.
Are nightmares a sign I should stop the medication?
Not on your own. Abruptly stopping certain meds can worsen sleep, trigger withdrawal, or cause serious medical problems. A supervised plantiming changes, slower titration, or a within-class switchis usually safer than stopping cold turkey.
What if I have PTSD, sleep apnea, or I’m acting out my dreams?
PTSD can increase nightmare frequency, and treatments like Imagery Rehearsal Therapy can help nightmares tied to trauma [Aurora et al., 2010]. Sleep apnea can fragment sleep and amplify dream recall, treating it can reduce nightmare-like awakenings. Acting out dreams can suggest REM sleep behavior disorder, which should be evaluated promptly [AASM, 2014].
Is melatonin from supplements safer than prescription options for nightmares?
Melatonin can help some circadian-related sleep issues, but it can also increase vivid dreams for some people, and supplement doses/quality vary. If nightmares began after adding melatonin, include it in your log and discuss itespecially if you take other sedating meds.
When should I see a doctor (or sleep specialist) about nightmares?
Seek evaluation if nightmares last more than a few weeks, happen multiple times per week, cause you to avoid sleep, or impair daytime functioning/safety. Go urgently for nightmares that signal danger if you’re acting out dreams, have hallucinations/confusion, or the nightmares involve self-harm thoughts (or you wake up with those thoughts lingering) [AASM, 2014].
The bottom line
Medication-related nightmares are common, often fixable, and extremely miserable at 4 a.m. The move is: stay safe, gather a little data, and ask for targeted changesinstead of suffering or rage-quitting a medication you genuinely need.
Go fight for your sleep. Politely. Safely. With a notebook.
Sources
- American Academy of Sleep Medicine. International Classification of Sleep Disorders (ICSD-3). 2014. (reference text)
- Aurora RN, Zak RS, Auerbach SH, et al. “Best practice guide for the treatment of nightmare disorder in adults.” Journal of Clinical Sleep Medicine, 2010. (guideline)
- Qaseem A, Kansagara D, Forciea MA, Cooke M, Denberg TD. “Management of Chronic Insomnia Disorder in Adults: A Clinical Practice Guideline From the American College of Physicians.” Annals of Internal Medicine, 2016. (guideline)
- Wilson S, Argyropoulos S. “Antidepressants and sleep: a qualitative review of the literature.” Drugs, 2005. (review)
- Thompson DF, Pierce DR. “Drug-induced nightmares.” The Annals of Pharmacotherapy, 1999. (review)
- U.S. Food & Drug Administration (FDA). Donepezil (Aricept) Prescribing Information (abnormal dreams/nightmares listed). https://www.accessdata.fda.gov/ (drug label)
- U.S. Food & Drug Administration (FDA). Varenicline (Chantix) Prescribing Information (abnormal dreams/vivid dreams listed). https://www.accessdata.fda.gov/ (drug label)
- U.S. Food & Drug Administration (FDA). “FDA strengthens warning that malaria drug mefloquine may cause neuropsychiatric side effects.” 2013. https://www.fda.gov/ (safety communication)
- Department of Veterans Affairs/Department of Defense. VA/DoD Clinical Practice Guideline for the Management of Posttraumatic Stress Disorder and Acute Stress Disorder. 2023. (guideline)
- Raskind MA, Peskind ER, Chow B, et al. “Trial of Prazosin for Post-Traumatic Stress Disorder in Military Veterans.” New England Journal of Medicine, 2018. (clinical trial)