You’re careful with your neck all day after surgery, but sleep is a different story. Your body moves unconsciously at night, often into positions your surgeon warned against, which is why many patients wake up sore despite following daytime instructions.
This guide explains how to sleep after cervical neck surgery with practical positioning techniques, equipment tips that actually work, and realistic week-by-week expectations.
You’ll learn the setup details most discharge instructions skip, troubleshooting for common sleep problems, and how to distinguish normal healing discomfort from signs that need medical attention.
By the end, you’ll have a clear plan for protecting your neck while getting the rest your body needs to heal.
The Real Reasons Sleeping Hurts After Cervical Surgery
Here’s what nobody explains well about how to sleep after cervical neck surgery: you’re incredibly careful during the day. You avoid sudden movements.
You protect your neck. But at night? Your brain shuts off that caution. You unconsciously roll onto your stomach. You crank your head to the side.
You tuck your chin or hyperextend backward, all the movements your surgeon warned against. This gap between daytime awareness and nighttime carelessness is why you wake up in worse pain than when you went to bed.
Your surgical site is healing, but your sleeping habits are working against it.
What You Should Know about Surgeries
Before you leave the hospital, clarify these specifics. Generic discharge instructions skip the details that make or break your first week of sleep.
- Some surgeries require a 30-45° incline for the first week to reduce swelling. Others don’t. Know your number.
- Some surgeons want 24/7 brace wear for 6 weeks. Others say remove it at night after week one. Wrong assumptions here cause panic at 2 am.
- Minor position shifts won’t ruin your surgery. Sudden forceful rotation or hyperextension during a fall is the real risk.
- Rolling onto your side in week three won’t pop your fusion. This fear keeps patients rigid and sleepless for no reason.
Multi-level surgeries usually need stricter positioning longer than single-level.
Safe Sleeping Positions After Cervical Surgery
Most blogs preach back-sleeping like it’s gospel. Here’s reality: the best position is the one that keeps your neck neutral and lets you actually sleep. Here’s how each option works.
| Position | Why It Works | Setup | Common Mistake |
|---|---|---|---|
| Back with incline (default for most) | Gravity reduces swelling; no rotation stress | Wedge pillow or adjustable base at 30-40°; thin pillow under head for neutral alignment | Pillow too high, folds neck forward |
| Side sleeping (after clearance, usually week 3+) | Easier for habitual side sleepers once inflammation settles | Pillow fills shoulder-to-ear gap; knees bent with pillow between them to prevent torso twist. | Upper shoulder rolling forward rotates the neck |
| Recliner (short-term only) | Useful week one when getting in/out of bed is brutal | Add lumbar cushion; knees slightly elevated | Using the past week two, wrecked my lower back |
| Stomach | Never. Forces extreme rotation. | Never. | Never |
How to Get In and Out of Bed Without Wrecking Your Neck
Getting in and out of bed requires careful technique because even one wrong twist can strain your recovering neck and delay healing by several weeks.
1. Getting in Bed
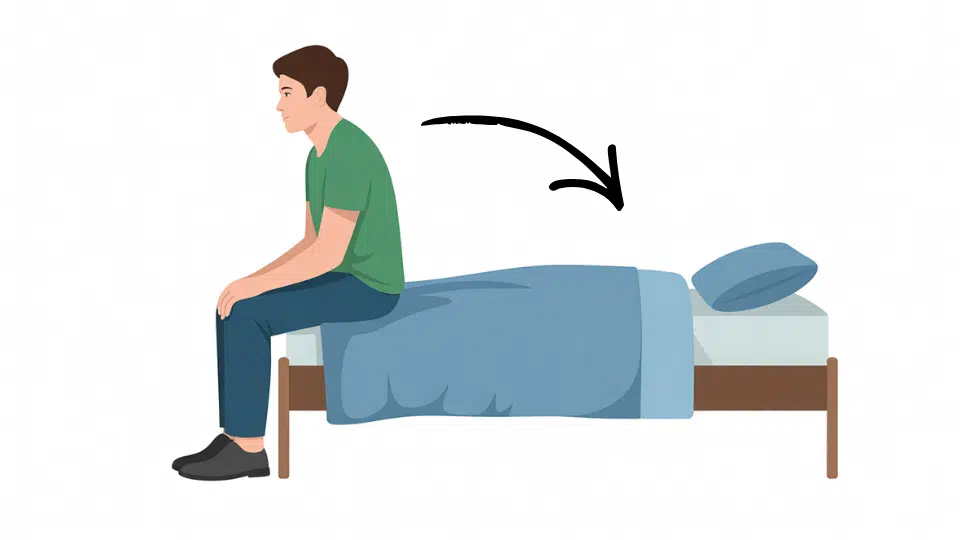
Sit on the edge with hips positioned where you want them when lying down. Lower your torso sideways as one unit, keeping shoulders, ribs, and hips moving together.
Use your arms to control descent, not your neck muscles. Your head should be the last thing to touch the pillow, landing already aligned. Choose a bed height where feet touch the floor when sitting for better control.
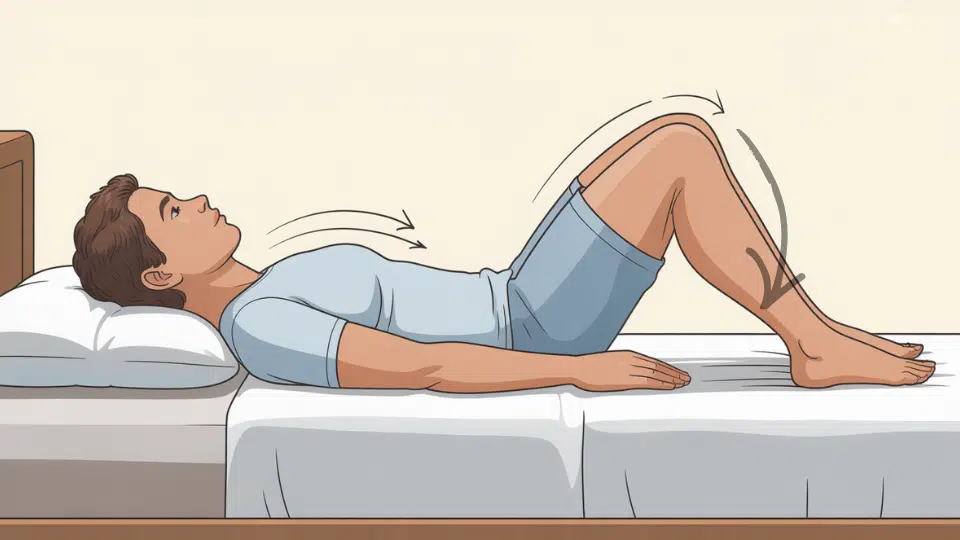
2. Changing Sides During the Night

Bend your knees first if you need to roll over. Push with your legs and core to rotate your entire body at once.
Keep your nose pointing in the same direction as your chest and avoid looking around while you move. Use your forearms for stability, not to push your head up.
3. Getting out of Bed
Roll onto your side as one unit, then pause briefly. Push up with your bottom arm while simultaneously swinging your legs off the bed.
Your head should stay in line with your spine the entire time. Sit on the edge for a few seconds before standing to avoid dizziness or strain.
Pillows, Braces, and Equipment, and What Actually Matters
Forget brand recommendations. Here’s how to self-assess whether what you have is working.”
- Pillow height test: Lie down and have someone check from the side. Your ear should align with your shoulder, nose pointing straight up, not angled toward the ceiling (pillow too low) or tucked to your chest (too high). Most people need less height than they think.
- When to use a wedge: If nerve pain or arm tingling worsens when flat, a 30-40° incline can take pressure off. But if you wake with mid-back pain, the angle is too steep, or you need lumbar support.
- Sleeping in a cervical collar: Tighten just enough that it doesn’t shift when you move, not so tight you can’t swallow comfortably. If the edges dig into your skin, pad with soft fabric. If you’re waking with worse pain in the brace, it may be fitted wrong; call your surgeon’s office.
Do you need a “cervical pillow”? Only if it achieves neck neutrality. A rolled towel under your neck curve often works better than a $150 contour pillow that props your head too high.
What to Expect Week by Week
Recovery isn’t linear. Most online timelines are too optimistic. Here’s what actually happens in each phase, plus red flags that mean call your surgeon immediately.
| Timeline | Sleep Reality | Red Flag |
|---|---|---|
| Week 1-2 | Terrible sleep. You’ll wake frequently from pain, brace discomfort, or fear of moving. This is normal. | New severe pain, sudden arm weakness |
| Week 3-4 | Slightly better. You’ll find one tolerable position. Still stiff in the mornings. | Increased tingling, pain spreading to new areas |
| Week 6-8 | Gradual improvement. Most patients can sleep 4-5 hours straight. | Still can’t tolerate any position, fever, or wound drainage |
| Week 8+ | Return to near-normal (if cleared by surgeon). Some morning stiffness may linger for months. | Balance loss, bladder/bowel changes |
Your timeline may vary slightly based on your procedure type and overall health. But if you’re hitting the red flags, don’t wait, call your surgeon.
Troubleshooting When Sleep Keeps Going Wrong
If you’re following all the rules but still waking in agony, work through these common culprits before assuming something’s wrong with your surgery.
Worse pain in the morning?
- The pillow is probably too high. Lower it by one inch and retest. Check if your brace shifted, tighten or pad the edges.
Waking on your stomach?
- Place a body pillow in front of you to block the unconscious roll.
Arms tingling at night?
- Mild tingling that resolves when you move is typical nerve irritation. Worsening tingling with weakness, call your surgeon.
Can’t tolerate back sleeping?
- Try 45° semi-recline instead of flat. If nothing works after two weeks, tell your surgeon it may signal swelling.
Meds disrupting sleep?
- Ask about earlier evening dosing. Never adjust doses yourself.
Most sleep problems stem from pillow height or positioning. But persistent issues despite adjustments deserve a conversation with your surgeon’s office.
Red Flags that need medical attention
If you experience any of these symptoms, don’t wait until morning; contact emergency medical services right away.
| Red-Flag Symptom | Description |
|---|---|
| New severe pain | Pain that feels different from your baseline surgical pain |
| Sudden arm or hand weakness | Trouble holding objects, dropping things, or a loose grip |
| Loss of balance or coordination | Difficulty walking steadily or feeling uncoordinated |
| Loss of bladder or bowel control | Inability to control urination or bowel movements |
| Fever over 101°F | High fever or fluid leaking from the incision site |
| Difficulty swallowing or breathing | Especially common concern after anterior cervical procedures |
| Worsening tingling/numbness | Sensations spreading to new areas or getting progressively worse |
Your Before-Bed Checklist
- Take pain medication 30-45 minutes before bed if prescribed on schedule
- Brace check: fitted comfortably, edges not digging in, not shifting loose
- Pillow height test: lie down and verify ear aligns with shoulder when on your back
- Gather essentials within arm’s reach: phone, water, medications, TV remote on nightstand
- Five-minute wind-down: gentle walk around your room or slow breathing practice
- Room prep: cool temperature, dark, minimal noise
- Skip neck stretches, your surgeon will clear those later
The Bottom Line
Recovery sleep won’t feel normal for weeks. The positioning techniques, equipment adjustments, and movement strategies here protect the surgical site while finding tolerable positions.
Some nights will be difficult even with correct setup,healing tissue and irritated nerves at work. But there’s a difference between expected discomfort and warning signs needing medical attention.
Trust the timeline, follow red flag guidelines, and remember: the surgeon cleared this because healing potential outweighs temporary sleep disruptions. The body needs time.
Want more recovery guidance? Read our complete guide to cervical surgery rehabilitation and daily activity modifications.