Last updated: 2025-12-23
Educational content only — not medical advice.
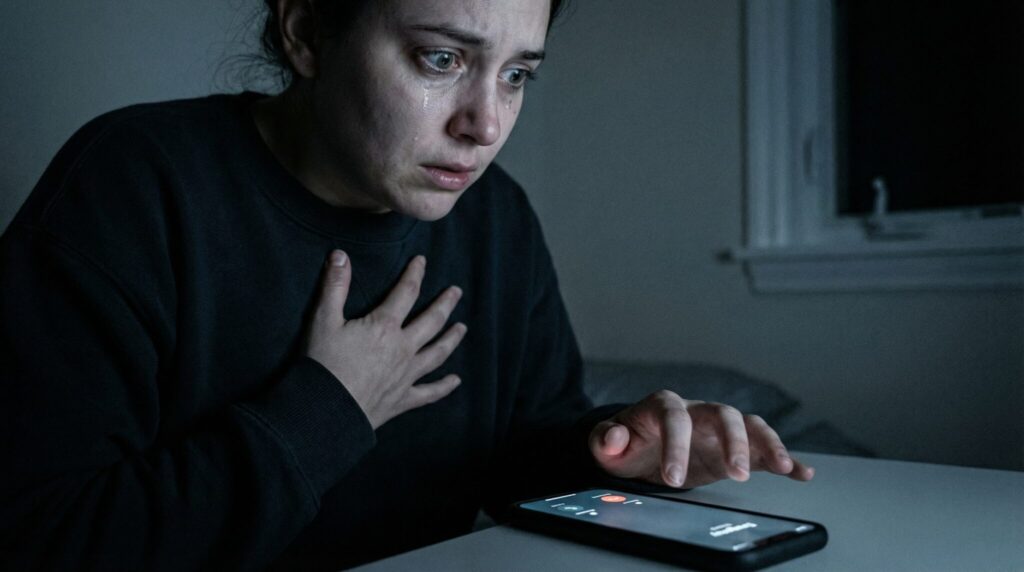
When your body is screaming “WE ARE IN DANGER” and your brain is like, “Okay but… are we, though?” yep. That specific flavor of terror is awful.
And honestly? It’s also common. A lot of people end up in the ER because the physical symptoms of panic (racing heart, chest tightness, can’t breathe feeling) can feel indistinguishable from a real medical emergency.
The short answer: If symptoms are new, severe, or include red flags (spreading chest pressure, fainting, stroke signs, blue lips, severe trouble breathing), treat it as an emergency and call your local emergency number.
Key exception: If you know you get panic attacks and this episode is clearly identical and improving with time/grounding, you may be able to monitor at home but panic and medical problems can overlap.
When it matters less: If you’ve been evaluated before for similar episodes and nothing dangerous was found, you can focus more on a “panic plan” and follow up care while still taking any new or different symptoms seriously.
Before we go any further: I’m not your clinician, and this isn’t medical advice. This is the “here’s a clear plan when your nervous system is acting like a smoke alarm” post. If you’re not sure, it is always okay to get checked.
First: What a Panic Attack Usually Feels Like (and Why It’s So Convincing)
A panic attack often hits fast like someone slammed the “ALERT” button in your chest for no apparent reason.
Common panic symptoms include:
- pounding or racing heartbeat
- chest tightness
- shortness of breath / air hunger
- sweating, shaking, chills or hot flashes
- nausea, dizziness, “I might pass out”
- tingling or numbness (often hands/face)
- feeling unreal or detached
- a sudden certainty that something terrible is happening
The reason it feels so intense is because your body can dump stress hormones and flip into fight or flight… even if you’re literally just standing in your kitchen staring at a cereal box. Clinically, panic attacks are defined as a sudden surge of intense fear/discomfort with physical symptoms that peak within minutes for many people [American Psychiatric Association, DSM-5-TR].
The timeline clue (helpful, but not a “rule”)
A typical panic attack often:
- rises quickly
- peaks within minutes (commonly around ~10 minutes)
- then eases over the next 20-60 minutes
But: panic can come in waves, can last longer, and timing alone can’t rule out heart/lung problems. Use this as a supporting clue, not a diagnostic test [American Psychiatric Association, DSM-5-TR].
If the timing is way off or things aren’t easing at all or symptoms are new/different that’s a strong reason to stop assuming it’s “just anxiety.”
The “What Do I Do Right Now?” Checklist
When you’re scared, you don’t need a pep talk. You need a decision tree.
Call emergency services immediately if you have ANY of these
(US/Canada: 911. EU/UK and many countries: 112. Use your local emergency number.)
- chest pressure/pain that spreads to your arm, jaw, neck, or back [AHA/ACC Chest Pain Guideline, 2021]
- crushing/squeezing chest discomfort, especially if it lasts more than a few minutes or comes with sweating/nausea [AHA/ACC Chest Pain Guideline, 2021]
- severe shortness of breath, gasping, or breathing that’s getting worse (especially at rest)
- blue/gray lips or face, or you can’t stay awake
- fainting, near fainting, new confusion, seizure, or a “this is the worst I’ve ever felt” sense
- stroke signs: face drooping, one sided weakness/numbness, slurred speech, sudden severe confusion [CDC Stroke Signs (FAST)]
- severe allergic reaction signs: swelling of lips/tongue/throat, widespread hives, wheezing/stridor, repetitive vomiting, or collapse [World Allergy Organization Anaphylaxis Guidance, 2020]
- pulmonary embolism (blood clot) red flags: sharp chest pain that’s worse with breathing, coughing blood, new one sided leg swelling/pain, or recent surgery/immobility/postpartum/hormone therapy + sudden shortness of breath [ESC Pulmonary Embolism Guideline, 2019]
- aortic dissection red flags: sudden, severe “tearing/ripping” chest or back pain, or chest pain with new neurologic symptoms or fainting [ACC/AHA Aortic Disease Guideline, 2022]
- chest pain/palpitations after cocaine/amphetamines, or severe alcohol/benzo withdrawal symptoms (shaking, confusion, seizures)
Go to the ER now (and don’t drive yourself if you feel faint) if:
- this is your first ever episode with chest pain, significant palpitations, or shortness of breath
- symptoms are staying severe and not improving at all, or you’re deteriorating
- you feel better and then get a clear second surge that’s intense or different
- you have higher risk history (known heart disease, pregnancy/postpartum, significant asthma/COPD, clot risk, prior fainting with palpitations) [AHA/ACC Chest Pain Guideline, 2021; ESC Pulmonary Embolism Guideline, 2019]
Consider urgent care / same day clinic / telehealth if:
- you’re not having red flags, but symptoms are newish, changing, or you’re unsure
- you need help deciding what level of care fits today (many insurers and health systems have 24/7 nurse lines)
Important: urgent care is often not the right place for significant chest pain, severe breathing trouble, fainting, or stroke/allergy symptoms those need an ER (or an ambulance).
Stay home and monitor if ALL of these are true:
- you have a known history of panic attacks and this matches your usual pattern
- no red flags from the lists above
- grounding/breathing tools are helping at least a little
- intensity is trending down over time (even if it’s still unpleasant)
Follow up within 24-48 hours if:
- episodes are becoming frequent, more intense, or changing
- you went to the ER and need a prevention plan
- you’re not in immediate danger, but you’re scared and unsure what’s driving this
Quick triage table (save this)
| Best next step | When it fits best | Don’t use it if… |
|---|---|---|
| Call emergency services | Red flags (spreading chest pressure, fainting, stroke signs, severe allergic reaction, severe breathing trouble, suspected clot/dissection) | You’re trying to “wait it out” despite severe/worsening symptoms |
| Go to the ER now | First ever severe episode, not improving, major risk factors, symptoms feel medically “off” | You’re too faint/confused to travel safely (call emergency services) |
| Urgent care / same day / telehealth | No red flags, but you need evaluation or guidance today | Significant chest pain, severe shortness of breath, neuro symptoms, anaphylaxis signs |
| Home + monitor | Clearly typical panic pattern + improving + no red flags | Symptoms are new, different, escalating, or you’re unsure |
Two quick “reality checks” you can do at home (NOT diagnostic)
These can support your decision, but they cannot rule out emergencies. People with serious conditions can sometimes still speak, and people with panic can sometimes feel extremely breathless.
1) The “breathing is functional?” check
Try to say one full sentence out loud, like:
“I’m having symptoms and I’m trying to decide if I need help.”
- If you’re too breathless to speak, breathing is noisy, or you feel like you’re about to pass out: treat it as an emergency.
- If you can speak: that can be reassuring, but it’s not a guarantee you’re safe.
2) The “trend” check (instead of a strict clock test)
Note the time and watch the direction of symptoms:
- Are things slowly easing, even a little?
- Or are they flat lined at “max intensity,” worsening, or adding new symptoms?
If you’re not improving at all, or you’re getting worse, escalate.
“Okay, but what if it’s not panic?”
Here’s the frustrating truth: even ER clinicians often need exams, EKGs, and labs to tell the difference between panic and problems like heart disease, arrhythmias, asthma/COPD flares, blood clots, etc. Chest pain evaluation is specifically designed to avoid missing dangerous causes [AHA/ACC Chest Pain Guideline, 2021].
A few patterns that sometimes help (again: not rules):
- Chest pain type: panic discomfort can be sharp, shifting, or tied to hyperventilation. Heart related pain is more often heavy pressure/squeezing and may radiate [AHA/ACC Chest Pain Guideline, 2021].
- Heart rhythm: panic can be fast, but if your heartbeat feels irregular and you have dizziness/near fainting, that deserves urgent evaluation.
- Breathing response: if slowing your breathing reduces symptoms even a bit, panic is more likely. If you truly cannot get air, treat it as urgent.
Extra note for women (because bodies love to be “unique” at the worst times)
Heart symptoms can show up as heart attack warning signs like jaw/back pain, nausea, unusual sweating, crushing fatigue, or shortness of breath without classic chest pain [AHA/ACC Chest Pain Guideline, 2021]. If you have risk factors and you feel off in a new way, take that seriously.
Who should be extra cautious with “assume it’s panic”
- Pregnancy/postpartum (especially the first 6-12 weeks): clot risk is higher. Sudden shortness of breath, chest pain with breathing, or fainting should be evaluated urgently [ESC Pulmonary Embolism Guideline, 2019].
- Asthma/COPD: wheezing, chest tightness, or breathlessness can mimic panic. If rescue inhalers aren’t helping or you’re struggling to talk, escalate.
- Diabetes or frequent low blood sugar: shakiness, sweating, pounding heart, and anxiety can overlap with hypoglycemia. Check glucose if you can, and treat lows per your plan (and seek urgent care if severe/confusing).
- New meds/substances: decongestants, stimulants (including ADHD meds), thyroid meds, caffeine, cannabis, cocaine/amphetamines, and withdrawal from alcohol/benzodiazepines can cause dangerous symptoms err on the side of medical evaluation.
- History of heart disease, arrhythmia, clots, or fainting: have a lower threshold to get checked.
If you’re pretty sure it’s panic: what to do while it burns out
If you’re in the “this matches my usual panic pattern” category, here are a few tools that can change the trajectory. Pick one. Don’t try to do all of them at once.
1) Breathing (simple + bossy)
- Box breathing: inhale 4, hold 4, exhale 4, hold 4
- Or 4-7-8: inhale 4, hold 7, exhale 8
If counting makes you mad, just slow the exhale. A longer exhale can help shift your nervous system toward “safe enough.”
2) Grounding (the 5-4-3-2-1 thing that feels cheesy until it works)
Name:
- 5 things you see
- 4 things you can touch
- 3 things you hear
- 2 things you smell
- 1 thing you taste
3) Progressive muscle relaxation
Tense and release muscle groups starting at your feet and moving up.
If you try these for 10-15 minutes and nothing changes or you’re getting worse that’s a reason to seek care. Many panic episodes shift at least a little with time + nervous system cues, but not always.
When in doubt, don’t tough it out.
If you go to the ER: what it’ll probably look like (so it’s less scary)
If you walk in saying “I think this might be panic but I’m scared it’s my heart,” you are not wasting anyone’s time. Panic is often a diagnosis of exclusion they have to rule out dangerous causes first [AHA/ACC Chest Pain Guideline, 2021].
What they’ll ask
- your symptoms and when they started
- medical history + family history
- medications/supplements
- substance use (be honest this is clinical safety information)
- whether this matches past panic attacks
Common tests (depends on symptoms/risk)
- EKG
- bloodwork (often includes troponin for heart strain/injury)
- sometimes chest X-ray, thyroid labs, urine tests
- if clot risk is a concern: D-dimer and/or CT imaging [ESC Pulmonary Embolism Guideline, 2019]
If everything dangerous is ruled out and it looks like panic, you’ll usually get reassurance, coaching for breathing/grounding, and sometimes a short acting medication for acute distress (case by case).
How to describe symptoms so you’re clear (and fast)
Try:
- where the pain is and what it feels like (pressure? stabbing? burning?)
- whether it spreads to arm/jaw/back
- whether you feel faint/confused
- what’s different from your usual panic pattern (if you have one)
- any big risk factors (pregnancy/postpartum, heart disease, clot history, recent surgery/immobility, stimulant use, etc.)
After the storm: how to keep this from running your life
The temptation after a panic episode is to treat it like a bad dream and pretend it didn’t happen. I get it. But future you deserves a plan.
Follow up timing I like
- Within 24-48 hours: primary care visit (bring ER paperwork if you went)
- Within 1-2 weeks: ask about therapy and/or psychiatry if panic is recurring
Treatments that actually work (not just “try to relax”)
- CBT (Cognitive Behavioral Therapy): especially panic focused CBT (including interoceptive exposure) is a first line treatment in major guidelines [NICE CG113].
- SSRIs/SNRIs: commonly used for panic disorder. They take weeks to build benefit and should be guided by a clinician [NICE CG113].
- Benzodiazepines: can reduce acute distress, but carry dependence/withdrawal risks and are generally used cautiously and short term (clinician guided) [NICE CG113].
The boring lifestyle stuff that matters more than it should
Sleep, less caffeine, regular movement, lowering alcohol/nicotine these can all nudge your baseline arousal down.
Make a “Panic Plan” while you’re calm (seriously, do it once)
When panic hits, your brain is not in spreadsheet mode. So set this up in advance:
- a note on your phone with: meds, diagnoses, allergies, emergency contact, and any past heart workups
- your “usual” panic pattern (how it starts, how long it tends to last, what helps)
- one support person you can call to sit with you, time the episode, and help decide if you should escalate
- crisis contacts saved (US):
- 988 Suicide & Crisis Lifeline (call/text)
- Crisis Text Line: text HOME to 741741
Frequently Asked Questions
Should I go to the ER for a panic attack?
Go to the ER (or call emergency services) if symptoms are new, severe, different from your usual, or include red flags like spreading chest pressure, fainting, stroke signs, severe breathing trouble, or signs of an allergic reaction. Panic can feel identical to emergencies, and sometimes both can happen together. When you’re unsure, choosing safety is reasonable.
Can a panic attack cause chest pain and shortness of breath?
Yes panic attacks commonly cause chest tightness, rapid heart rate, and air hunger. That said, chest symptoms are also a top sign of heart/lung emergencies, so don’t use “it might be panic” to talk yourself out of urgent care when something feels medically wrong [AHA/ACC Chest Pain Guideline, 2021].
How long can a panic attack last?
Many peak within minutes and ease within about an hour, but some come in waves or feel prolonged. Timing can support your decision making, but it can’t reliably distinguish panic from medical problems [American Psychiatric Association, DSM-5-TR].
Should I call 911 or drive myself?
Call emergency services if you might pass out, you’re severely short of breath, you have neurologic symptoms (stroke signs), or you have severe chest pressure or collapse risk. If you’re going to the ER but feel faint or unsafe to drive, get a ride or call for help don’t “white knuckle” a drive.
Are there risks to doing breathing exercises if this isn’t panic?
Gentle breathing and grounding are generally safe, but the risk is delay: feeling a bit better doesn’t prove you’re not having a heart, lung, or allergic emergency. If red flags are present or symptoms are worsening, seek care first.
Is “food/supplement melatonin / magnesium / herbs” a substitute for treating panic?
Not really. Supplements may help some people with sleep or anxiety, but they’re not an acute triage tool and can interact with medications. For recurrent panic, evidence based treatments like panic focused CBT and appropriate medications tend to have stronger support [NICE CG113].
When should I seek professional help for panic or anxiety (even if I don’t go to the ER)?
See a healthcare professional if panic attacks are recurring, you’re avoiding normal activities, you’re using alcohol/drugs to cope, you have suicidal thoughts, or symptoms persist most days for more than a few weeks. Seek urgent evaluation sooner if you’ve had fainting, chest pain with exertion, repeated nighttime gasping/choking, or daytime sleepiness that makes driving/work unsafe.
The bottom line (the part I want you to remember)
If something feels new, severe, or “wrong” in a way you can’t explain get checked. Never be embarrassed for choosing safety. ERs exist for uncertainty.
And if it is panic? You’re not broken. Your body is overprotective. Check the trend, take one slow exhale, and do the next right thing.
Sources
- Gulati M, Levy PD, Mukherjee D, et al. “2021 AHA/ACC/ASE/CHEST/SAEM/SCCT/SCMR Guideline for the Evaluation and Diagnosis of Chest Pain.” Circulation, 2021. (guideline)
- Centers for Disease Control and Prevention (CDC). “Stroke Signs and Symptoms (FAST).” https://www.cdc.gov/stroke/signssymptoms.htm (overview)
- Cardona V, Ansotegui IJ, Ebisawa M, et al. “World Allergy Organization Anaphylaxis Guidance 2020.” World Allergy Organization Journal, 2020. (guideline)
- Konstantinides SV, Meyer G, Becattini C, et al. “2019 ESC Guidelines for the diagnosis and management of acute pulmonary embolism.” European Heart Journal, 2019. (guideline)
- Isselbacher EM, Preventza O, Hamilton Black J III, et al. “2022 ACC/AHA Guideline for the Diagnosis and Management of Aortic Disease.” Circulation, 2022. (guideline)
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM-5-TR). APA Publishing, 2022. (reference)
- National Institute for Health and Care Excellence (NICE). “Generalised anxiety disorder and panic disorder in adults: management (CG113).” https://www.nice.org.uk/guidance/cg113 (guideline)