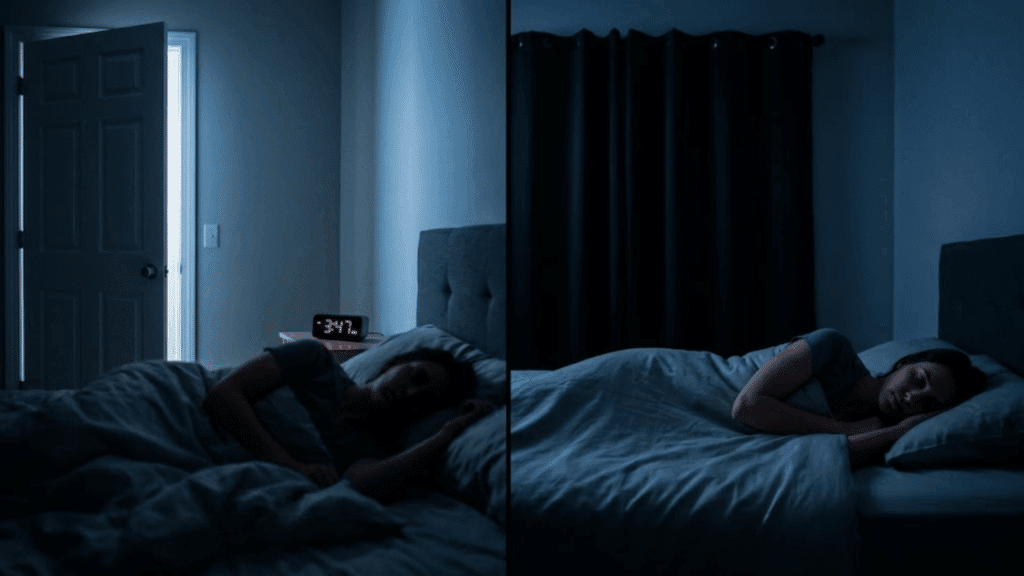
I used to think waking up once or twice during the night was just part of getting older.
Turns out, I was experiencing fragmented sleep, repeated awakenings that prevent you from completing full sleep cycles. If you’re constantly hitting snooze or struggling to focus during the day, you’re not alone.
Studies show that fragmented sleep affects millions of people, quietly chipping away at memory, mood, and even long-term heart health.
Once I understood what was disrupting my sleep, I found practical ways to reclaim those precious, uninterrupted hours. Let me share what actually works.
What is Fragmented Sleep?
Fragmented sleep occurs when you experience repeated brief awakenings or arousals throughout the night, preventing you from completing full, restorative sleep cycles, even if you spend enough time in bed.
Here’s how it differs from other sleep issues:
- Fragmented Sleep: You wake up multiple times during the night, disrupting your sleep architecture despite adequate time in bed
- Insomnia: You struggle to fall asleep initially or stay asleep, often lying awake for extended periods, feeling frustrated
- Sleep Deprivation: You simply don’t allocate enough hours for sleep, whether by choice or circumstance
Understanding these distinctions helps you identify the root cause and find the right solution for better rest.
How Common is Fragmented Sleep?
Fragmented sleep is surprisingly widespread, though it often goes unrecognized.
Research indicates that older adults experience it most frequently; up to 60% of people over 65 report multiple nighttime awakenings due to age-related changes in sleep architecture.
Shift workers face similar challenges, with irregular schedules disrupting their circadian rhythms and leading to frequent arousals.
People with obstructive sleep apnea (OSA) are particularly vulnerable, experiencing dozens or even hundreds of brief awakenings per night as their breathing repeatedly stops and starts.
Even among healthy adults, studies suggest that 35-40% occasionally experience fragmented sleep, whether due to stress, environmental factors, or lifestyle habits that disrupt continuous rest.
Major Causes of Fragmented Sleep
Fragmented sleep rarely happens without reason. From underlying sleep disorders to everyday habits, multiple factors can interrupt your night’s rest.
Understanding what’s causing your awakenings is the first step toward solving them.
1. Sleep Disorders
Obstructive sleep apnea (OSA) is one of the most common culprits; your airway repeatedly collapses during sleep, causing brief awakenings as your body struggles to breathe.
You might not even remember these micro-arousals, but they severely disrupt sleep quality.
Periodic limb movement disorder and restless legs syndrome also fragment sleep by causing involuntary leg movements or uncomfortable sensations that jolt you awake throughout the night, preventing deep, restorative rest.
2. Medical Conditions & Pain
Chronic conditions frequently interrupt sleep patterns. GERD causes nighttime heartburn that wakes you gasping or coughing.
Nocturia, the need to urinate multiple times nightly, becomes more common with age and certain medical conditions.
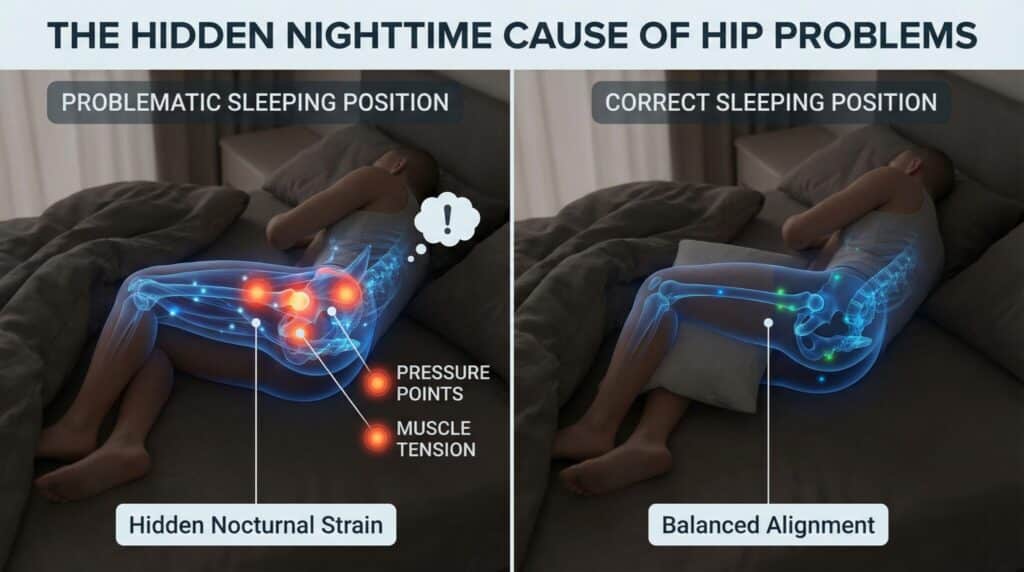
Chronic pain from arthritis, fibromyalgia, or back problems makes it nearly impossible to stay comfortable long enough to complete full sleep cycles, creating a frustrating cycle of brief rest followed by painful awakenings.
3. Lifestyle and Behavioral Causes
Your daily habits significantly impact nighttime sleep continuity.
Alcohol might help you fall asleep initially, but fragments your sleep in the second half of the night. Late-afternoon caffeine lingers in your system for hours.
Irregular sleep schedules, especially shift work or “social jetlag” from weekend sleep pattern changes, confuse your body’s internal clock, making it difficult to sleep continuously even when you’re exhausted.
4. Environmental Causes
Your sleep environment matters more than you think. Noise from traffic, neighbors, or a snoring partner can trigger brief awakenings.
Light exposure, even from street lamps or device indicators, disrupts melatonin production. A room temperature that’s too warm or too cold prevents deep sleep.
Partners with different schedules, restless pets, or young children frequently interrupt your rest, creating patterns of fragmented sleep that persist even after the disruptions stop.
5. Medication & Substance Effects
Certain medications paradoxically interfere with sleep quality. Stimulants obviously disrupt rest, but some antidepressants alter sleep architecture. Beta-blockers can reduce melatonin production.
Sedatives might help initially, but often cause rebound awakenings as they wear off. Corticosteroids, decongestants, and some asthma medications also fragment sleep.
If you started a new medication around the time your sleep problems began, that connection is worth exploring with your doctor.
6. Psychological Causes
Mental health significantly impacts sleep continuity. Anxiety keeps your mind hypervigilant, causing frequent awakenings as your brain remains alert for threats.
PTSD commonly causes nightmares and sudden awakenings with a racing heart and sweaty palms. Chronic stress elevates cortisol levels throughout the night, preventing the deep relaxation necessary for uninterrupted sleep.
Depression can also fragment sleep patterns, creating both early-morning awakenings and difficulty maintaining continuous rest.
Short- and Long-Term Effects of Fragmented Sleep
When your sleep gets repeatedly interrupted, the consequences ripple through every aspect of your health, from how you function the next day to your risk of developing serious chronic diseases years down the road.
| Impact Category | Immediate Effects | Long-Term Consequences | Key Research Findings |
|---|---|---|---|
| Daily Function | Severe daytime sleepiness, impaired concentration, and mood swings | Increased accident risk, reduced productivity | Fragmented sleep causes more sleepiness than equal total sleep deprivation |
| Brain Health | Memory deficits, poor decision-making, and emotional dysregulation | Depression and anxiety, cognitive decline risk | Causes oxidative stress damage in the hippocampus, affecting memory |
| Physical Health | Weakened immunity, raised stress hormones, metabolic disruption | Cardiovascular disease, type 2 diabetes, and chronic inflammation | Increases leukocyte production, accelerating atherosclerosis |
The Bottom Line: Fragmented sleep prevents your body from completing restorative processes that only happen during uninterrupted sleep cycles, creating both immediate impairment and long-term disease risk.
How is Fragmented Sleep Diagnosed?
Diagnosing fragmented sleep starts with tracking your patterns. Sleep diaries documenting bedtime, wake times, and nighttime awakenings provide crucial baseline data.
Your doctor may also use validated questionnaires like the Epworth Sleepiness Scale to assess daytime impairment and calculate sleep efficiency metrics.
For suspected sleep disorders, home sleep apnea tests offer convenient, cost-effective screening for straightforward cases of obstructive sleep apnea.
In-laboratory polysomnography remains the gold standard, measuring brain waves, breathing, heart rate, and limb movements to identify causes of sleep fragmentation, like periodic limb movements or sleep-stage disruptions, that home tests miss.
When to See a Sleep Specialist? Seek evaluation if you experience loud snoring, breathing pauses, daytime sleepiness despite 7+ hours, morning headaches, difficulty concentrating, or unexplained mood changes.
12 Evidence-Based Strategies to Reduce Sleep Fragmentation

The good news: most causes of fragmented sleep can be addressed with targeted interventions.
If your interruptions stem from a medical condition, lifestyle habits, or environmental factors, these evidence-based strategies can help you reclaim uninterrupted rest.
1. Treat Underlying Sleep Disorders
If you have obstructive sleep apnea, CPAP therapy dramatically reduces nighttime awakenings by keeping airways open. For periodic limb movement disorder, medications or iron supplementation (if deficient) can quiet restless legs.
Don’t try to diagnose yourself; a sleep specialist can identify the root cause and prescribe appropriate treatment that actually addresses the problem.
2. Keep a Consistent Sleep-Wake Schedule
Your body’s internal clock thrives on predictability. Going to bed and waking up at the same time every day, yes, even weekends, strengthens your circadian rhythm and consolidates sleep.
Irregular schedules confuse your brain about when to release sleep-promoting hormones, leading to more frequent awakenings and lighter sleep throughout the night.
3. Optimize Your Sleep Environment
Create a sleep sanctuary: pitch dark (use blackout curtains), quiet (try white noise or earplugs), and cool, ideally 60-67°F (15-19°C). Even small amounts of light can disrupt melatonin production and fragment sleep.
Temperature matters too; your body needs to cool slightly to maintain deep sleep, so a warm bedroom triggers more awakenings.
4. Reduce Evening Stimulants and Alcohol
Caffeine has a half-life of 5-6 hours, so that 3 PM coffee still affects you at bedtime. Cut off caffeine by early afternoon.
While alcohol might help you fall asleep initially, it fragments sleep in the second half of the night as your body metabolizes it, causing frequent awakenings.
5. Limit Late Fluids and Manage Nocturia
Nighttime urination disrupts sleep continuity for millions. Stop drinking fluids 2-3 hours before bed.
If you still wake frequently to urinate, talk to your doctor; medications like diuretics taken too late or underlying conditions like diabetes may be contributing. Timing adjustments can make a significant difference.
6. Try CBT-I and Relaxation Techniques
Cognitive behavioral therapy for insomnia specifically addresses anxiety-driven awakenings and teaches sleep maintenance skills.
Techniques like progressive muscle relaxation, deep breathing, and mindfulness meditation calm an overactive nervous system. Unlike sleeping pills, CBT-I provides lasting improvements without side effects or dependency risks.
7. Exercise Regularly (but Time It Right)
Regular physical activity improves sleep quality and reduces nighttime awakenings. However, vigorous exercise within 2-3 hours of bedtime can be stimulating for some people.
Morning or afternoon workouts are ideal; they help regulate your circadian rhythm while giving your body time to wind down before bed.
8. Address Bedroom Partner Issues
A snoring or restless partner can fragment your sleep without you fully realizing it. Solutions include earplugs, separate blankets to prevent tug-of-war, or even temporary, separate sleeping arrangements.
If your partner snores loudly, encourage them to get evaluated for sleep apnea; treatment benefits you both.
9. Review Medications With Your Doctor
Certain medications fragment sleep as a side effect: stimulants, some antidepressants, beta-blockers, corticosteroids, and decongestants.
Don’t stop medications on your own, but ask your doctor if alternatives exist or if timing adjustments might help. Sometimes a simple switch from nighttime to morning dosing resolves the issue.
10. Strategies for Shift Workers
If you work irregular hours, strategic 20-minute naps before shifts, bright light exposure during work hours, and physician-supervised melatonin timing can help.
Keep your sleeping space extremely dark during daytime sleep and maintain the same sleep schedule on days off when possible to minimize circadian disruption.
11. Manage Pain Effectively
Chronic pain and sleep fragmentation create a vicious cycle. Work with your doctor on multimodal pain control: physical therapy, anti-inflammatory medications, topical treatments, and positioning aids.
Addressing pain before bed, rather than waiting until it wakes you, prevents interruptions and improves overall sleep architecture.
12. Track Your Progress and Adjust
Use a sleep diary or wearable device to monitor patterns: bedtime, wake time, number of awakenings, and how you feel. After implementing changes for 2-3 weeks, review your data.
If fragmentation persists despite consistent efforts, consult a sleep specialist for professional evaluation and personalized treatment.
When Fragmentation Can’t Be Fixed With Lifestyle Alone
Sometimes lifestyle changes aren’t enough. CPAP or BiPAP therapy effectively treats obstructive sleep apnea by maintaining open airways throughout the night. Oral appliances offer an alternative for mild to moderate cases.
For periodic limb movement disorder, iron therapy (if deficient) or medications can reduce nighttime movements.
Sleep medications provide short-term relief but carry risks of dependency and rebound insomnia; use them cautiously under medical supervision.
Cognitive behavioral therapy for insomnia (CBT-I) offers lasting benefits without medication side effects.
If standard treatments fail, your sleep specialist may refer you to an ENT for surgical evaluation or recommend advanced therapies tailored to your specific diagnosis.
Monitoring Improvement: Metrics That Matter
Track the right indicators to know if your interventions are working. Give changes at least 2-4 weeks before evaluating progress; sleep patterns take time to shift.
- Sleep Efficiency: Aim for 85% or higher (total sleep time divided by time in bed)
- Number of Awakenings: Track frequency and duration of nighttime interruptions
- Time in Deep and REM Sleep: Quality matters as much as quantity
- Daytime Sleepiness: Use the Epworth Sleepiness Scale to measure functional improvement
- Subjective Sleep Quality: How rested you feel matters more than any device reading
If you see no improvement after 4 weeks of consistent effort, consult a sleep specialist for professional guidance.
Real-Life Examples of Sleep Fragmentation
Seeing how others have successfully addressed fragmented sleep can provide hope and practical insights. Here are two evidence-based examples from published research showing different paths to better sleep.
Case 1: Sleep Apnea Resolved With CPAP
A 53-year-old male patient with severe obstructive sleep apnea experienced 40+ awakenings per hour, severe daytime sleepiness, and morning headaches.
After starting CPAP therapy, his sleep fragmentation decreased by over 50% within the first month.
His arousal index dropped dramatically, slow-wave sleep increased by 56%, and his Epworth Sleepiness Scale score improved from 18 (severe) to 6 (normal). He reported feeling refreshed for the first time in years.
Case 2: Anxiety-Driven Insomnia Improved With CBT-I
A middle-aged woman with chronic insomnia and anxiety spent hours awake worrying about not sleeping, creating a self-perpetuating cycle.
Through six sessions of cognitive behavioral therapy for insomnia, she learned sleep restriction techniques, stimulus control, and cognitive reframing.
After treatment, she fell asleep easily and slept soundly through the night. She described her results: “I have no anxiety about not sleeping. My body gets signals it’s time to sleep and I’m confident about sleep now.”
Final Thoughts
Fragmented sleep doesn’t have to be your permanent reality. I’ve shown you the causes, consequences, and science-backed solutions to reclaim continuous, restorative rest.
If your fragmentation stems from sleep apnea, anxiety, lifestyle habits, or environmental factors, targeted interventions can make a meaningful difference.
Start with one or two strategies that resonate most with your situation, track your progress for a few weeks, and adjust as needed.
Have you tried any of these approaches? What’s worked (or hasn’t worked) for your fragmented sleep?
Share your experience in the comments below; your insights might help someone else finally get the uninterrupted sleep they desperately need.