Sometimes snoring seems harmless, but if you’ve ever woken up gasping or short of breath, it might be a warning sign you shouldn’t ignore.
Sleep apnea can quietly strain your heart and body night after night. You might wonder, can sleep apnea kill you, or is it just an inconvenience?
In this guide, I’ll walk you through what really happens during sleep apnea, how it can become dangerous, and the steps you can take to stay safe.
You’ll learn how to spot the warning signs early, understand your treatment options, and take control of your health before this condition leads to something serious.
Can Sleep Apnea Kill You?
Yes, sleep apnea can be deadly if it’s left untreated. Every pause in breathing drops your oxygen level, forcing your heart to work harder to keep blood flowing.
Over time, this constant strain can lead to:
- Heart failure
- Stroke
- Dangerous heart rhythms that can turn fatal during sleep
You might wonder, How fast can sleep apnea kill you? It depends on how severe it is and whether you’re treating it.
- In many people, the damage builds slowly over years of poor oxygen and broken sleep.
- In severe, untreated cases, a single night of deep oxygen loss can trigger a fatal event without warning.
The longer it goes untreated, the higher the risk becomes, but with proper treatment, the danger can drop dramatically, and your breathing can return to normal.
What Happens Inside Your Body During Sleep Apnea
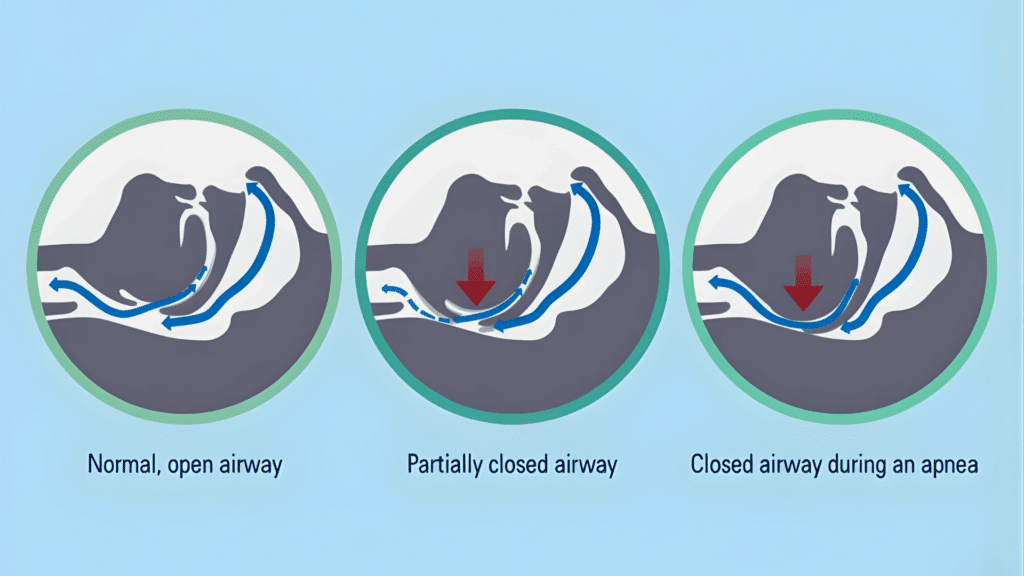
Each time your airway closes, your oxygen level drops, and your body reacts instantly. Your brain senses the lack of oxygen and sends a distress signal that briefly wakes you up just enough to reopen your airway.
You may not remember it, but this can happen dozens or even hundreds of times each night.
These constant interruptions stop you from reaching deep, restorative sleep. Instead, your body stays in a state of stress, flooding your system with hormones like adrenaline and cortisol.
Over time, this stress causes real physical damage:
- Blood pressure rises because your body stays alert even while you sleep.
- Blood thickens, making it harder for your heart to pump efficiently.
- The heart weakens from the repeated strain of oxygen drops and pressure spikes.
- Blood sugar and metabolism can shift, raising the risk of diabetes and weight gain.
It’s a silent cycle that slowly wears down your heart, brain, and overall energy levels. Without treatment, your body never truly rests, and the effects build night after night.
Types of Sleep Apnea and Their Risks
Not all sleep apnea is the same. Each type affects your breathing differently and carries its own level of danger.
1. Obstructive Sleep Apnea (OSA)
This is the most common type. It happens when throat muscles relax too much and block the airway. Oxygen levels drop, your brain jolts you awake, and the cycle repeats all night.
Over time, OSA puts pressure on your heart and blood vessels, leading to high blood pressure, heart rhythm problems, stroke, or even sudden death during sleep if untreated.
2. Central Sleep Apnea (CSA)
With CSA, your brain temporarily stops sending signals to breathe. The body “forgets” to take a breath, causing longer and deeper oxygen drops than in OSA.
It’s often connected to heart or nervous system problems and can lead to severe fatigue, confusion, and dangerous heart rhythm changes.
3. Complex or Mixed Sleep Apnea
This type combines both obstructive and central features. It can appear during CPAP treatment or develop on its own, making management more difficult.
OSA blocks airflow, CSA disrupts brain control, and complex apnea mixes both. Identifying the right type is key to choosing effective treatment and preventing serious complications.
Key Risk Factors for Sleep Apnea
Some people are more likely to develop sleep apnea or face serious complications. Here’s a quick look at the main risk factors and why they matter:
| Risk Factor | Why It Raises Risk |
|---|---|
| Men over 40 | Men tend to carry more fat around the neck and have narrower airways. Hormones and age-related muscle loss make blockages more likely. |
| Obesity or a large neck | Extra tissue around the throat can block airflow, especially when lying flat. |
| Heart disease or high blood pressure | Oxygen drops during sleep add more strain to an already stressed heart. |
| Alcohol or sedative use | These relax the throat muscles and slow the brain’s response to low oxygen. |
| Untreated severe OSA or CSA | Long-term oxygen loss puts major stress on the heart and can become life-threatening. |
If any of these apply to you, it’s best to get tested early; sleep apnea is far easier to control once it’s diagnosed.
Sleep Apnea Warning Signs You Shouldn’t Ignore
Sleep apnea often goes unnoticed, but your body sends out warning signals. Watch for:
- Loud, ongoing snoring that disturbs others
- Gasping or choking sounds during sleep
- Waking up unrefreshed or with a dry mouth
- Morning headaches or light-headedness
- Chest discomfort or uneven heartbeat after waking
- Severe daytime fatigue or trouble staying alert
If these symptoms sound familiar, don’t wait to get checked. Sleep apnea can quietly progress from mild to life-threatening, often without clear warning.
How Sleep Apnea is Diagnosed?

Getting diagnosed is the most important step toward safe, effective treatment. Because sleep apnea symptoms often appear only during sleep, testing is the only reliable way to confirm it.
Doctors use two main methods depending on your symptoms and health history.
1. Home Sleep Test
A home sleep test (HST) is a simple, at-home way to check for obstructive sleep apnea. Your doctor gives you a small device to wear overnight that records:
- Airflow through your nose and mouth
- Oxygen levels in your blood
- Breathing effort and pauses
- Heart rate while you sleep
The test is comfortable, affordable, and works well for people who have mild to moderate symptoms or no major medical complications.
A home test doesn’t measure brain activity, so it can’t detect when you’re fully asleep or distinguish between obstructive and central sleep apnea. If your results are unclear or your doctor suspects a more complex case, an in-lab study is the next step.
2. In-Lab Sleep Study (Polysomnography)
An in-lab sleep study, also called polysomnography, is the gold standard for diagnosing all types of sleep apnea. It’s done overnight at a certified sleep center under the supervision of trained technicians.
During the study, sensors monitor multiple body functions, including:
- Brain waves (EEG): to measure sleep stages and disruptions
- Eye and muscle movements: to track REM and non-REM cycles
- Heart rhythm (ECG): to detect irregular beats during apnea events
- Oxygen and airflow sensors: to record drops in oxygen and pauses in breathing
- Body position and leg movements: to identify positional or movement-related issues
After the study, a sleep specialist analyzes the data to determine:
- The number of breathing pauses per hour (Apnea-Hypopnea Index or AHI)
- How severe the oxygen drops were
- What type of sleep apnea is present (obstructive, central, or complex)
A home test works for simpler cases, but an in-lab study provides deeper insights, helping doctors choose the safest and most effective treatment for you.
How Treatment Can Prevent Death?
Treating sleep apnea doesn’t just improve sleep; it prevents life-threatening complications. The options below help keep your airway open, stabilize oxygen, and protect your heart.
| Treatment Option | How It Helps | Key Notes |
|---|---|---|
| CPAP and PAP Therapy | Keeps the airway open and oxygen steady throughout the night. | Lowers the risk of heart disease, stroke, and sudden death. Consistent use is critical for results. |
| Oral Devices & Positional Therapy | Custom dental devices or side-sleeping reduce airway collapse. | Useful for mild to moderate apnea or for those who can’t tolerate CPAP. |
| Lifestyle Changes | Improves breathing stability and heart health. | – Maintain a healthy weight – Avoid alcohol and sedatives – Quit smoking – Sleep 7+ hours a night Even small changes can extend lifespan. |
| CPAP Safety & Recalls | Addresses potential equipment issues. | Some devices were recalled in 2021 due to foam-related risks. Always check your device’s status and never stop therapy without medical guidance; the benefits far outweigh the risks. |
Sleep apnea treatment saves lives. Whether through CPAP, oral devices, or healthier habits, keeping your airway open protects your heart and prevents sudden, fatal events.
Simple Prevention Checklist for Sleep Apnea
Small daily habits can make sleep apnea easier to manage and lower the risk of serious complications:
- Sleep on your side: Lying on your back can block your airway, while side-sleeping keeps it open and reduces pauses in breathing.
- Raise your head slightly: A supportive pillow or mild incline helps air move freely and prevents throat collapse.
- Avoid alcohol or heavy meals before bed: Both relax throat muscles and make apnea worse. Stop eating or drinking alcohol at least two hours before sleep.
- Keep a steady sleep routine: Going to bed and waking up at the same time helps your body maintain regular breathing patterns.
- Clean your CPAP often: Regular cleaning prevents bacteria buildup and keeps airflow steady for safe, effective therapy.
- Stay active and manage weight: Exercise strengthens breathing muscles and reduces pressure on the airway. Even modest weight loss can improve symptoms.
These simple steps support your treatment, improve sleep quality, and greatly reduce your chances of heart problems or sudden complications from sleep apnea.
Summing Up
Now that you know the facts, it’s clear that sleep apnea is more than a sleep issue; it’s a real health risk. Asking can sleep apnea kill you isn’t dramatic; it’s an important question that can push you to take action before things get worse.
If you’ve been snoring, waking up tired, or gasping for air, it’s worth talking to your doctor. A simple test and steady treatment plan can make a huge difference in your safety and quality of life.
For more practical tips and honest advice on sleep and health, check out the other posts on my website.









